A radiologist struggles to discern faint micro-calcifications on a standard clinical display, knowing the diagnosis hangs in the balance. The screen, perfectly adequate for a CT scan, is failing this critical task.
Mammography must visualize tiny, low-contrast targets like micro-calcifications, demanding superior spatial resolution, luminance, and grayscale uniformity. CT imaging, focused on broader anatomical structures and density trends, is more forgiving of display variations.
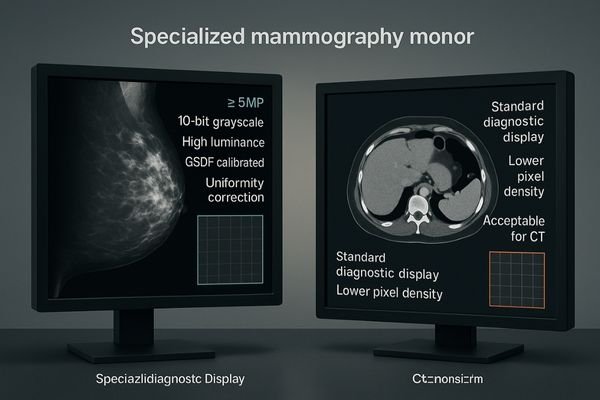
In any radiology department, not all images are created equal, and neither are the displays used to interpret them. While both mammography and computed tomography (CT)1 are essential diagnostic tools, the nature of the information they present places different demands on the viewing system. A display that provides a clear, diagnostically sound view of a CT scan may be inadequate for interpreting a mammogram. The reason lies in the clinical objective: mammography searches for minuscule, subtle signs of early-stage cancer, whereas CT often focuses on larger anatomical relationships and tissue density changes. This difference means the technical specifications for a mammography display—from pixel density to luminance stability—must be held to a stricter standard.
Why is mammography stricter?
Comparing the display needs of mammography and CT is like comparing the tools of a watchmaker to those of a carpenter. Both are experts, but their tasks demand different levels of precision.
Mammography requires visualization of micro-calcifications and subtle tissue distortions, demanding the highest spatial resolution, luminance, and low-noise grayscale performance. CT is more tolerant, as it emphasizes larger anatomical structures.
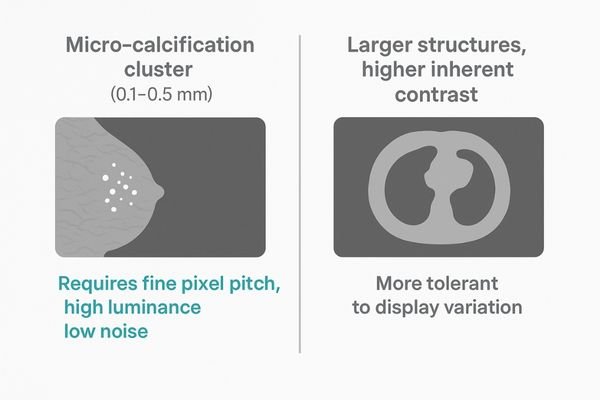
The stringency of display requirements for mammography comes from the nature of early-stage breast cancer. The primary targets—micro-calcifications2—can be a few tenths of a millimeter with very low contrast against surrounding tissue. Detecting these indicators requires a display system that resolves extremely fine details without introducing noise or artifacts that could obscure them. This is a question of both spatial resolution and grayscale fidelity.
Spatial vs. Density Resolution
A mammography display needs a very small pixel pitch so tiny calcifications are not lost to pixelation. It also needs high luminance and a carefully calibrated Grayscale Standard Display Function (GSDF) to make faint, low-contrast structures visible. By contrast, CT’s primary diagnostic information often comes from differentiating density in larger organs and tissue structures. Findings are generally larger and have higher inherent contrast than micro-calcification clusters. A standard diagnostic display can often render these differences without the extreme precision demanded by mammography. CT benefits from quality displays, but it is more robust to minor variations; mammography is acutely sensitive to even slight deviations.
Clinical impact: tiny differences, big decisions
On a mammography display, a barely noticeable variance in brightness or a single stuck pixel is not a minor annoyance. It is a potential source of a life-altering diagnostic error.
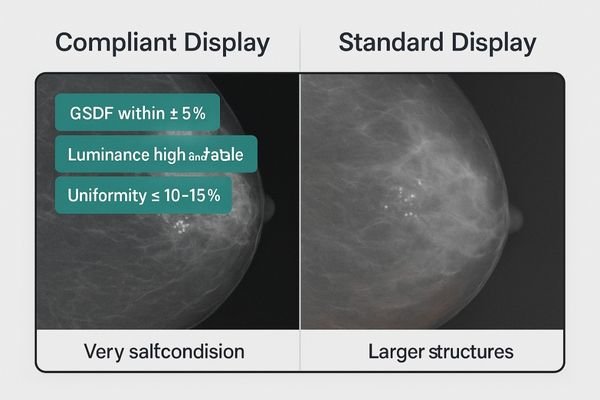
In mammography, even minor display flaws like insufficient luminance or GSDF errors can hide micro-calcifications or distort lesion margins, directly increasing the risk of false negatives or false positives.
The clinical stakes in mammography are high, and display quality is a direct variable in the diagnostic equation. A subtle deviation from required performance can affect decisions and outcomes.
The Risk of False Negatives
Insufficient luminance or GSDF errors can hide diagnostically significant findings. A cluster of faint micro-calcifications may fall below the perceptible threshold on a dim or poorly calibrated screen. This can lead to a false negative with serious consequences. Poor screen uniformity can also change the appearance of a lesion depending on its position, creating doubt and inconsistency.
False Positives and Patient Anxiety
Display artifacts may mimic pathology, leading to false positives3. A small cluster of dead pixels or a non-uniform bright spot could be misread as suspicious, triggering unnecessary anxiety, biopsies, and additional imaging. While CT interpretation also benefits from high-quality displays, the nature of CT findings makes them less vulnerable to such subtle variations.
Root causes: pixels, grayscale, uniformity, environment
The superior performance required for mammography is not a single feature but a combination of interdependent technical factors working together.
Mammography demands a finer pixel pitch, true 10-bit grayscale depth, and stricter uniformity. Panel aging, luminance drift, and ambient light leakage disproportionately impact the detectability of its subtle findings.
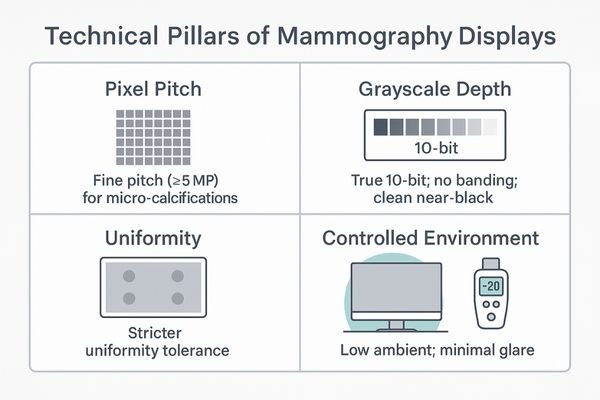
The stricter demands of mammography displays stem from four interconnected root causes: pixel characteristics, grayscale rendition4, panel uniformity, and environmental sensitivity.
Pixel Density and Grayscale Fidelity
Pixel pitch must be very fine to provide the spatial resolution needed to visualize micro-calcifications without aliasing. The display should support true 10-bit grayscale to render subtle shades and prevent banding that can mask texture. Low black-level noise is critical to keep near-black details clean.
Uniformity and Stability
Uniformity must be held to tighter tolerances than general radiology. A small brightness difference between center and corner can render a low-contrast mass invisible if it falls in a darker zone. Panel aging and luminance drift should be monitored and corrected continuously. Even small amounts of ambient light can introduce veiling glare, making controlled room lighting a requirement.
The solution: lock the chain to mammography needs
Ensuring diagnostic confidence in mammography requires an end-to-end ecosystem where every link is optimized for its demanding requirements.
Use high-resolution, mammography-grade diagnostic displays (5MP or higher) with integrated DICOM GSDF calibration, luminance stabilization, uniformity correction, and automated audit logs, paired with a controlled ambient light environment.
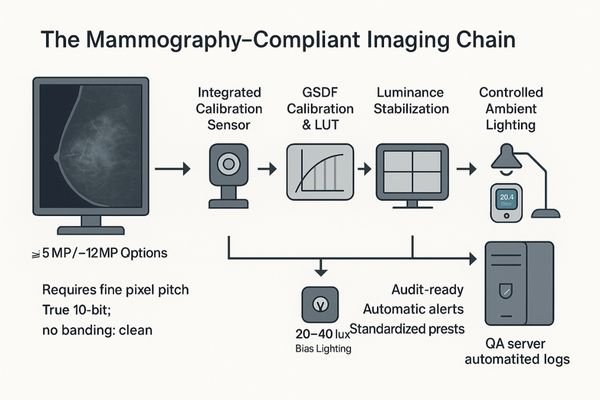
Build a closed-loop system in which hardware, software, and the environment are bound to mammography standards. Start with a mammography-grade display of at least 5MP; 8MP and 12MP offer more flexible layouts. Include continuous luminance stabilization, automated GSDF verification, and uniformity correction. Log all calibration and QA events to maintain a verifiable device history. Pair the display with controlled room lighting and locked reading presets to eliminate user-driven variability. The goal is consistent, objective output across time and operators.
Recommended Mammography-Grade Displays
| Model | Resolution / Size | 10-bit | GSDF & Auto-Cal | Luminance Stabilization | Uniformity Correction | Anti-Reflection | Primary Use Case |
|---|---|---|---|---|---|---|---|
| MD52G | 5MP / 21.3" | Yes | Yes | Yes | Yes | Yes | Traditional dual-head mammography and DBT |
| MD120C | 12MP | Yes | Yes | Yes | Yes | Yes | Single-screen workflow for DBT and fusion imaging |
| MD85CA | 8MP / 31.5" | Yes | Yes | Yes | Yes | Yes | Flexible multimodality reading including mammo |
Business value: higher detection, fewer disputes, audit-ready
Investing in specialized mammography displays is not an expense; it is a strategic investment in clinical excellence, operational efficiency, and risk management.
The value is clear: improved micro-calcification detection, fewer re-reads and medico-legal disputes, and streamlined QA processes that make the department perpetually audit-ready, strengthening its reputation and efficiency.
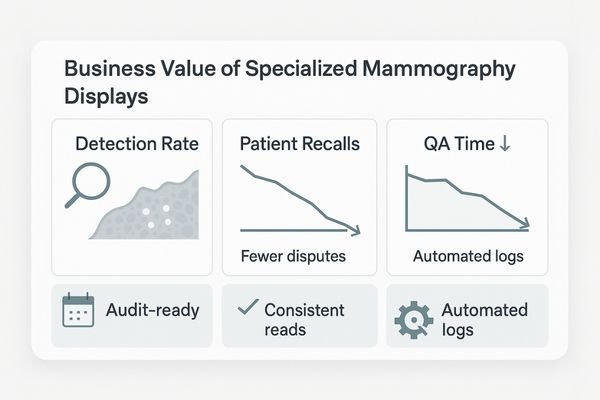
The decision to equip a mammography service5 with dedicated displays delivers returns across clinical, operational, and financial domains. Better tools improve detection and reduce recalls. Automated calibration and logging reduce manual workload for physics and IT. Audit-ready logs simplify accreditation preparation. Demonstrating technology leadership helps attract and retain clinical talent.
FAQ
Can mammography and CT scans be read on the same monitor?
Yes, on a unified multimodality platform. However, primary mammogram interpretation should use a 5MP or higher display with dedicated mammography presets and controlled lighting. CT can share the platform in different layouts with appropriate settings.
Is a single manual calibration sufficient for a mammography display?
No. Given mammography’s sensitivity, one-time calibration is inadequate. Continuous luminance stabilization, automated DICOM GSDF verification, and active uniformity correction are required. All activities should be recorded in traceable logs to keep the device compliant between manual checks.
Is an 8MP or 12MP display better than a traditional dual 5MP setup?
It depends on workflow. Dual 5MP is a proven and efficient configuration for mammography. Single 8MP or 12MP displays provide a larger field of view and convenient multimodality, provided pixel density, grayscale performance, and calibration still meet mammography standards.
Conclusion
Use mammography’s strict display thresholds as the benchmark for your department. Lock GSDF, luminance, uniformity, 10-bit, and room lighting into a consistent QA loop to deliver reliable, high-fidelity results across mammography and CT. 🩻
👉 For expert support and Reshin’s diagnostic display solutions, contact info@reshinmonitors.com.
-
Exploring the differences between CT and mammography can enhance your understanding of their unique diagnostic capabilities. ↩
-
Understanding micro-calcifications is crucial for early breast cancer detection. Explore this link to learn more about their significance. ↩
-
Exploring false positives helps in recognizing the psychological impact on patients and the importance of accurate imaging. ↩
-
Exploring grayscale rendition can reveal its critical role in enhancing image quality and diagnostic accuracy in mammography. ↩
-
Explore this link to understand how dedicated displays enhance mammography services, improving detection and operational efficiency. ↩



