Relying on a non-specialist display for mammography risks missing subtle micro-calcifications. This compromises diagnostic accuracy and creates inconsistencies between readings, undermining the core purpose of breast cancer screening.
This guide defines the “best” 5MP mammography monitor not by peak specs, but by its fitness for breast imaging. We will cover the critical criteria: DICOM-true grayscale, sustained high luminance, uniformity, and seamless workflow integration.
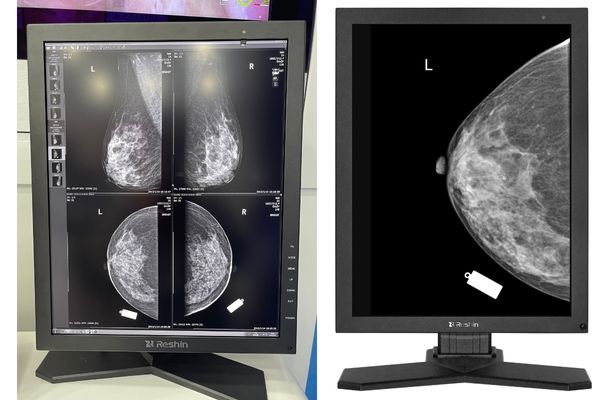
- Reshin MD52G — 5MP monochrome; DICOM-true grayscale, stabilized luminance, high uniformity; ideal for DBT.
- Barco Nio Color 5MP (MDNC-6121) — 5MP color for mixed color/mono workflows; high luminance; enterprise QA ecosystem.
- EIZO RadiForce GX560 — 5MP monochrome; precise grayscale, uniformity correction, long-term stability.
When evaluating a 5MP monitor for mammography and digital breast tomosynthesis (DBT), the ultimate goal is diagnostic confidence. This is not achieved by chasing the highest numbers on a specification sheet, but by ensuring the perceptual consistency of grayscale information every single day, across every workstation. The most important factors are strict adherence to the DICOM Part 14 standard1, the ability to sustain a high calibrated luminance over thousands of hours, and exceptionally tight screen uniformity2. These elements ensure that what a radiologist sees is a true representation of the patient’s anatomy, free from display-induced artifacts.
What “best” means for a 5MP mammography display in 2025 (selection criteria)
Defining the "best" display based on marketing claims can be misleading. Peak brightness or contrast ratios do not guarantee superior clinical performance in a demanding mammography environment.
For a 5MP breast imaging monitor, “best” is defined by unwavering task fitness. This means consistent grayscale perception day-to-day, a direct result of strict DICOM compliance, sustained luminance, and exceptional uniformity.
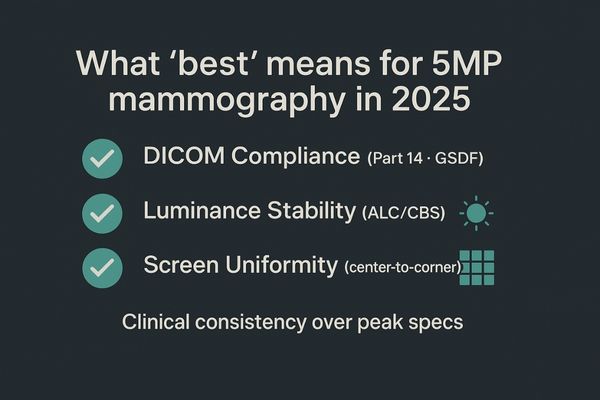
Our selection criteria prioritize clinical reality over abstract numbers. The most valuable 5MP display is one that maintains its calibrated performance3 over its entire lifecycle, ensuring that a prior study viewed five years ago looks perceptually identical to a new study viewed today. This requires a holistic approach to engineering. It starts with a panel capable of high brightness and contrast but is truly defined by the systems that manage that performance. These include a stabilization circuit to maintain calibrated luminance, a uniformity compensation engine to ensure the screen’s center and corners are visually identical, and an automated quality assurance system to verify DICOM Part 14 compliance4. This combination turns a high-performance panel into a trusted diagnostic tool, forming the foundation of our ranking logic. A display must prove its long-term stability to be considered among the best.
Ranking weights (how this list was scored)
- DICOM Part 14 adherence & auto-QC cadence — 30%
- Sustained calibrated luminance (DBT endurance) — 25%
- Screen uniformity (center-to-corner) — 20%
- Bit depth & LUT grayscale linearity — 15%
- Workflow & connectivity (dual-head, DP/DVI, EDID) — 10%
DICOM Part 14 for breast imaging: acceptance, tolerance and maintenance
A monitor that is only compliant on the day it is installed is a liability. Without continuous verification, its grayscale accuracy can drift, creating diagnostic uncertainty without any warning.
Initial DICOM Part 14 acceptance is just the start. The best displays provide daily assurance by automatically holding the GSDF within tight tolerances, with visible logs and on-screen status indicators.
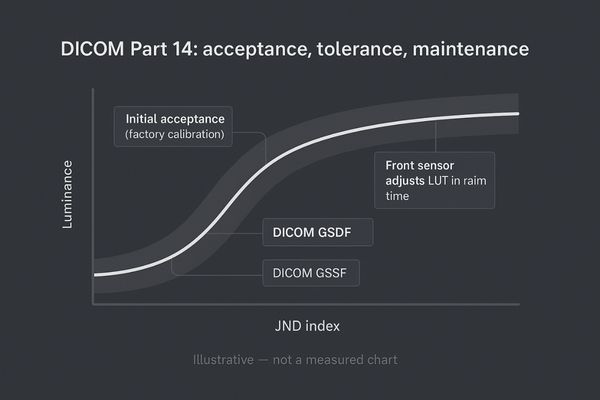
For mammography, adherence to the DICOM Part 14 Grayscale Standard Display Function (GSDF)5 is non-negotiable. This standard ensures that the relationship between pixel values in a digital image and the brightness levels on the screen is perceptually linear, allowing the human eye to distinguish subtle differences in tissue density. The process begins with an initial acceptance test to confirm the display meets the standard out of the box. However, the critical phase is maintenance. Environmental changes, backlight aging, and component wear can all cause a display to drift from its calibrated state. Superior 5MP monitors6 address this with built-in front sensors and automated QA software. This system performs regular checks without user intervention, adjusting the display’s look-up table (LUT) to maintain GSDF compliance. The results are logged for auditing, and a simple on-screen indicator provides the radiologist with immediate confidence that the display is performing as required. This transforms compliance from a periodic event into daily clinical assurance.
High luminance & stabilization (ALC/CBS): sustaining calibrated nits for DBT
High peak brightness is useless if it cannot be sustained. When reading DBT stacks, a fluctuating luminance level can cause eye fatigue and mask subtle details in the cine loop.
A high calibrated luminance, sustained by stabilization technologies like ALC, is essential for DBT. This ensures steady brightness over thousands of hours, reducing re-reads and improving diagnostic endurance.
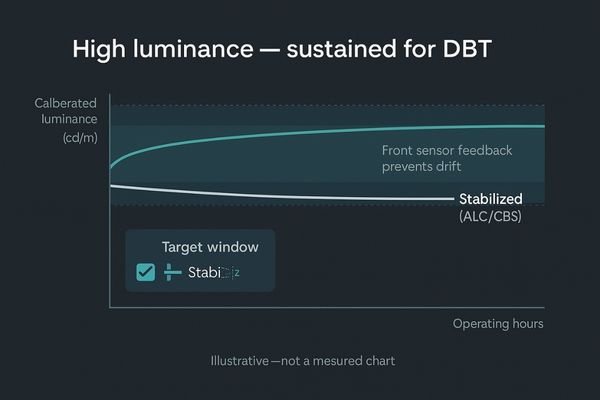
Digital Breast Tomosynthesis (DBT) places extreme demands on a display. As the radiologist scrolls through dozens of image slices, the monitor’s luminance must remain perfectly stable to ensure that a potential finding is equally visible on every slice. A high initial brightness of 1,000 cd/m² or more is required, but the ability to sustain that calibrated level is what truly matters. This is achieved through technologies often referred to as Automatic Luminance Control (ALC)7 or Constant Brightness Stabilization (CBS)8. These systems use a sensor to continuously monitor the backlight’s output and provide real-time feedback to the control circuitry, instantly compensating for any fluctuations. The result is a rock-solid brightness level that does not dim or flicker during long reading sessions or over the monitor’s lifespan. This feature, central to models like the MD52G, directly combats reader fatigue and ensures that diagnostic decisions are not influenced by inconsistent display performance, especially when reviewing demanding DBT datasets.
Uniformity & pixel pitch on 21.3": micro-calcification visibility across the screen
Screen non-uniformity is a clinical risk, not a cosmetic flaw. If the corners or edges of a display are dimmer than the center, a micro-calcification could appear less conspicuous or disappear entirely.
Superior uniformity compensation is critical for ensuring that micro-calcifications are equally visible anywhere on the screen. On a 21.3" 5MP panel, this is a core requirement for diagnostic confidence.

A standard 21.3-inch 5MP mammography display has a resolution of 2560×2048, resulting in a very fine pixel pitch. This high resolution is necessary to resolve tiny micro-calcifications8, which can be early indicators of malignancy. However, resolution alone is not enough. If the display’s brightness and color are not uniform from edge to edge, the conspicuity of these critical findings can change depending on their location on the screen. A lesion that is clearly visible in the brightly lit center might become ambiguous in a dimmer corner. To prevent this, premium diagnostic displays incorporate sophisticated uniformity compensation technology9. During manufacturing, the screen is measured at hundreds of points, and a correction map is created to adjust the brightness of individual pixel regions. This ensures that the entire screen area presents a single, consistent canvas, guaranteeing that a radiologist’s ability to detect pathology is never limited by the display’s physical properties.
| Feature | Importance for Micro-calcification Detection |
|---|---|
| 5MP Resolution | Provides the necessary pixel density to resolve individual calcifications. |
| Fine Pixel Pitch | Ensures sharp, clear rendering of the smallest structures. |
| Uniformity | Guarantees that the visibility of a finding is not dependent on its screen location. |
5MP Mammography Monitor Matrix (Quick Compare)
| Model | Panel | Size/Res | DICOM Auto-QC | Luminance (cal/peak) | Uniformity Comp. | Bit Depth/LUT | DP/DVI | Notes |
|---|---|---|---|---|---|---|---|---|
| Reshin MD52G | Monochrome | 21.3" 2560×2048 | Yes | High / High | Yes | 10/12-bit LUT | DP/DVI | DBT-ready, stable grayscale |
| Barco MDNC-6121 | Color | 21.3" 2560×2048 | Yes | High / — | Yes | 10-bit LUT | DP/DVI | Color/mono mixed workflows |
| EIZO GX560 | Monochrome | 21.3" 2560×2048 | Yes | High / — | Yes | 10-bit LUT | DP/DVI | Uniformity standout |
Bit depth, LUT & grayscale linearity: avoiding banding in dense breasts
A display with insufficient bit depth can introduce false contours. In dense breast tissue, this "banding" artifact can mimic or mask the subtle gradients that radiologists rely on for confident diagnosis.
A clean 10- or 12-bit grayscale pipeline and a medical-grade Look-Up Table (LUT) are essential for preventing banding artifacts and preserving the subtle density variations found in dense breast tissue.
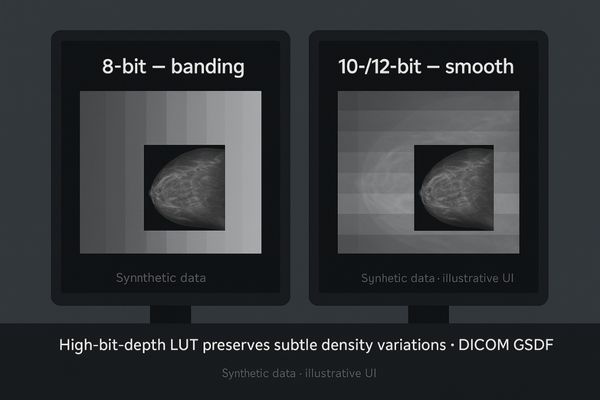
Mammography images, especially of dense breasts10, contain a wealth of information in subtle grayscale variations. An 8-bit display, capable of showing only 256 shades of gray, often lacks the fidelity to render these gradients smoothly. This can result in an artifact known as banding or contouring, where a continuous change in density appears as a series of distinct steps. To avoid this, high-end 5MP mammography monitors use a deeper bit depth in their internal processing. By using a 10-bit or 12-bit Look-Up Table (LUT), the monitor has access to 1,024 or even 4,096 shades of gray. This massive palette allows the display to select the optimal 256 shades (or more, depending on the panel) needed to create a perfectly smooth and linear grayscale ramp that is compliant with the DICOM GSDF11. This meticulous grayscale management ensures that the radiologist sees a faithful representation of the original image data, free of misleading artifacts.
Dual-head 5MP setups vs single-panel layouts: ergonomics and workflow
The choice between dual-head and single-panel setups can significantly impact workflow. While large single panels are available, the dual-head 5MP configuration remains the gold standard in mammography.
Dual-head 5MP pairs must function as identical twins. They require matched models and ages, synchronized calibration, and narrow bezels to ensure perceptual consistency and facilitate smooth eye movements.
The dual-head 5MP setup12 is deeply embedded in mammography workflow, primarily for comparing current and prior images or different views (like CC and MLO) side-by-side. For this comparison to be clinically valid, the two displays must be perceptually matched13. This means they should be the same model, ideally from the same production batch, and have a similar number of operating hours. Using mismatched models or ages can introduce subtle differences in brightness and color that disrupt diagnostic flow. Furthermore, both monitors must be calibrated together on the same schedule. Modern displays with narrow bezels are highly preferred, as they minimize the visual gap between the screens, allowing for smoother and less fatiguing eye movements (saccades) as the radiologist scans across the two images. While single wide-screen displays exist, the established workflow and perceptual assurance of a perfectly matched dual-head pair keep it the preferred choice for most breast imaging centers.
Connectivity that de-risks PACS integration: DP/DVI and EDID discipline
Intermittent signal loss during a reading session is unacceptable. Connectivity issues are a common source of frustration and downtime, often stemming from the use of adapters and poor signal negotiation.
To de-risk PACS integration, choose monitors with native DisplayPort and DVI connectivity. Proper EDID management prevents signal loss, and minimizing adapters reduces support tickets and speeds up deployment.

A 5MP display is a high-bandwidth device that requires a robust digital connection. The most reliable choices are native DisplayPort (DP)14 and dual-link DVI ports. Using these connections directly from the graphics card to the monitor eliminates a common point of failure: adapters. Adapters for HDMI or other standards can introduce signal integrity problems, leading to flickering, black screens, or a failure to achieve the full 5MP resolution. Another critical aspect of connectivity is Extended Display Identification Data (EDID)15. This is the information the monitor sends to the graphics card to report its capabilities. Poor EDID management can cause the workstation to send an incorrect signal. A quality medical display will have disciplined EDID programming, ensuring a stable handshake with the graphics card every time the system boots. By prioritizing native connections and solid EDID, a hospital can significantly reduce intermittent display issues and simplify the rollout and maintenance of PACS workstations.
| Port | Resolution Support | Recommended Use | Key Consideration |
|---|---|---|---|
| DisplayPort (DP) | High (5MP+ supported) | Primary Connection | Offers highest bandwidth and is the modern standard. |
| Dual-Link DVI | High (5MP supported) | Reliable Fallback | Robust and widely compatible with medical graphics cards. |
| HDMI / VGA | Variable (often <5MP) | Avoid for 5MP | Not designed for this resolution; requires adapters. |
Decision Checklist (Before You Buy)
- DICOM Part 14 + auto-QC schedule & logs
- Target calibrated luminance for DBT; stabilization present
- Center-to-corner uniformity within clinical tolerance
- 10/12-bit grayscale pipeline; medical LUT
- Dual-head ergonomics (matched pairs, narrow bezel)
- Native DP/Dual-link DVI; EDID discipline; minimal adapters
Conclusion
The best 5MP mammography monitor is one that delivers unwavering diagnostic confidence through stable, uniform, and DICOM-compliant performance over its entire lifespan. 🎯
👉 For trusted 5MP mammography solutions and expert support, contact martin@reshinmonitors.com.
-
Understanding the DICOM Part 14 standard is crucial for ensuring accurate imaging in mammography, enhancing diagnostic confidence. ↩
-
Exploring screen uniformity can reveal its impact on image quality, which is vital for accurate diagnoses in breast imaging. ↩
-
Understanding calibrated performance is crucial for ensuring consistent image quality over time, making it essential for diagnostic tools. ↩
-
Exploring DICOM Part 14 compliance will help you grasp its significance in medical imaging and the standards for display quality. ↩
-
Understanding GSDF is crucial for ensuring accurate mammography readings and improving patient outcomes. ↩
-
5MP monitors enhance image quality and compliance, essential for precise diagnostics in medical imaging. ↩
-
Understanding ALC can enhance your knowledge of display technologies crucial for medical imaging. ↩
-
Exploring CBS will reveal its importance in maintaining display quality for accurate diagnostics. ↩ ↩
-
Understanding this technology is crucial for ensuring accurate medical imaging and diagnosis. ↩
-
Understanding the challenges of dense breasts in mammography can enhance diagnostic accuracy and patient care. ↩
-
Exploring DICOM GSDF will provide insights into standards that ensure high-quality medical imaging and accurate diagnoses. ↩
-
Explore this link to understand the significance of dual-head 5MP setups in enhancing mammography workflows. ↩
-
Learn why perceptually matched displays are crucial for accurate diagnostics in mammography. ↩
-
Explore this link to understand why DisplayPort (DP) is essential for achieving optimal performance in high-resolution displays. ↩
-
Learn about EDID’s role in monitor performance and how it can prevent display issues in your setup. ↩



