Inconsistent image quality across different locations compromises remote diagnoses and care coordination. This can lead to misinterpretation, delayed decisions, and ultimately, a breakdown in the quality of patient care.
Medical-grade displays form the backbone of telemedicine: DICOM-compliant grayscale, stabilized luminance/uniformity, and low latency keep images identical across sites for teleradiology, virtual clinics, MDTs, and Tele-ICUs. Real-world programs show ~140% higher individual throughput and ~40% faster reporting with calibration and remote QA; as telemedicine expands from ~$100B (2024) toward $300B+ by ~2032 (CAGR ~16–17%), demand for high-standard displays will keep rising, enabling faster decisions and better outcomes.

The rapid expansion of telemedicine has permanently reshaped healthcare delivery, moving critical clinical functions beyond the hospital walls. From primary consultations to complex radiological reads and intensive care oversight, remote platforms depend on the flawless exchange of visual information. However, this virtual ecosystem is only as strong as its weakest link. Ensuring every clinician, regardless of location, sees the exact same image with identical detail and clarity is not just a technical goal—it is a clinical necessity. This is where medical-grade displays1 become the foundational technology, providing the calibrated, consistent, and compliant visualization required for confident remote decision-making. This article will explore the specific roles these displays play across various telemedicine applications2 and the technical standards that make them indispensable.
Remote diagnostics & reporting
Radiologists working remotely face the risk of diagnostic errors if their display cannot faithfully reproduce medical images. This inconsistency threatens both patient safety and professional confidence.
By ensuring DICOM compliance, stable luminance, and full-screen uniformity, medical-grade displays provide the perceptual consistency required for confident remote reading of CT, MRI, and X-ray studies.

The shift to remote radiology has been profound, with over 80% of radiology groups now permitting off-site reporting and more than 30% of radiologists reading primarily from home. This model’s success hinges entirely on maintaining diagnostic equivalence between the hospital reading room and the remote workstation. Medical-grade displays are the cornerstone of this equivalence. Their strict adherence to the DICOM Part 14 Grayscale Standard Display Function (GSDF)3 ensures that grayscale values are perceived identically, regardless of the device. Features like stabilized backlights and active uniformity correction guarantee that luminance is consistent across the entire screen and over time. This prevents subtle but critical findings from being lost in dimmer areas of the screen or due to performance drift. The impact is significant; sites that implement calibrated displays4 with structured remote quality assurance report remarkable efficiency gains, including up to 140% higher individual radiologist output and a 40% faster final report turnaround time, all without compromising diagnostic quality.
Virtual clinics & follow-ups
During virtual consultations, standard consumer webcams and monitors can distort subtle visual cues. This can lead to misjudgments of clinical signs like skin conditions or wound healing progress.
In video visits, medical-grade displays improve visual assessments of skin tone, rashes, and wound edges through superior color accuracy, higher bit depth, and a consistent white point.

The adoption of telemedicine for routine consultations skyrocketed from approximately 15% of physicians in 2019 to over 80% by 2021. In this context, the display screen becomes the primary tool for visual examination. A medical-grade display[^5 offers tangible advantages over a consumer model. Its higher bit depth allows for smoother color gradations, making it easier to accurately assess subtle variations in skin tone, the inflammation around a wound, or the specific characteristics of a rash. A factory-calibrated5, stable white point ensures that colors are rendered true-to-life, preventing the yellowish or bluish tint common on uncalibrated screens that could alter clinical perception. Furthermore, features designed for clinicians, such as wide viewing angles and the ability to seamlessly show side-by-side dashboards of patient data and video feeds, help reduce cognitive switching. This streamlined presentation improves focus on the
Multidisciplinary case conferences
When a virtual tumor board discusses a complex case, mismatched displays can cause clinicians to see different image details. This leads to debate over image quality rather than clinical strategy.
For virtual multidisciplinary teams, identical image presentation is paramount. Medical-grade displays with matched DICOM curves and synchronized brightness levels eliminate interpretation drift, fostering faster consensus.
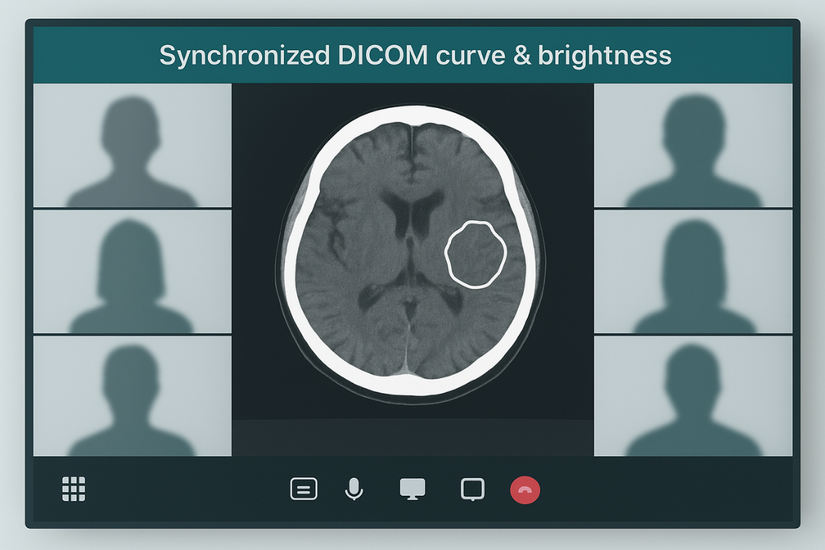
Virtual multidisciplinary team (MDT) meetings and tumor boards have become standard practice, with over 70% of participants expressing a desire to continue with the virtual format post-pandemic. The success of these conferences depends on a single, shared truth: every participant must see the exact same image. If one oncologist’s screen is brighter or has a different contrast curve than a radiologist’s, they may interpret the size or texture of a lesion differently. This is where medical-grade displays6 provide the critical infrastructure for collaboration. By ensuring that every display, adheres to the same DICOM calibration7, all participants perceive grayscale values identically. Centralized quality assurance tools can even synchronize brightness and other settings across all remote participants’ displays before a meeting begins. This technical alignment eliminates interpretation drift caused by hardware variables, allowing the team to focus on clinical analysis, reach a consensus more quickly, and reduce the need for follow-up meetings to clarify ambiguous findings.
Live telementoring & procedures
During remote procedural guidance, poor image quality can obscure critical anatomical details. This increases the risk of error for the operating surgeon and limits the effectiveness of the remote mentor.
For remote procedural mentoring, ultra-high-definition resolution and low latency on medical-grade displays are essential for rendering precise, real-time video feeds of instruments and anatomy without artifacts.

Telementoring allows experienced surgeons to guide their colleagues through complex procedures from anywhere in the world. This application demands flawless visual communication with near-zero delay. Medical-grade displays are engineered for this exacting environment. Their ability to render 4K and 8K video feeds, combined with advanced processing that ensures low latency, is critical. A delay of even a few milliseconds between the remote mentor’s instruction and the operating surgeon’s view can be disorienting. Furthermore, the high bit depth8 and superior color reproduction of these displays eliminate artifacts like color banding, ensuring that annotated lines and the fine tips of surgical instruments are rendered with absolute precision against complex anatomical backgrounds. Clinical centers that equip both the mentor and the mentee with calibrated, high-performance displays report tangible benefits, including shorter learning curves for new procedures and a notable reduction in aborted attempts due to technical visual limitations.
Centralized critical care
Monitoring dozens of ICU patients remotely from a central command center is an information-intensive task. Display flicker, instability, or non-uniformity can lead to missed alarms or misinterpreted data.
Tele-ICU programs rely on medical-grade displays to provide 24/7 stable, uniform luminance across multi-panel walls, ensuring critical vitals and imaging are read accurately for faster rescue decisions.

Tele-ICU programs9 have proven their ability to scale critical care expertise. In one large-scale program covering 15 ICUs, a central team conducted nearly 4,000 tele-rounds for over 5,000 patients in just 18 months. This "e-lCU" model relies on a command center where intensivists monitor multi-panel video walls displaying a constant stream of patient vitals, medical imaging, and bedside video feeds. The displays used in this environment must be exceptionally reliable. Medical-grade monitors are designed for 24/7 operation with stabilized backlights that prevent flicker or brightness drift over long hours. Their guaranteed screen uniformity ensures that a critical waveform or alarm displayed at the edge of a monitor is just as clear and visible as one in the center. This stability and consistency reduce the risk of misreading vital information during a crisis and enable the remote team to make faster, more confident decisions to intervene when a patient’s condition deteriorates.
Imaging fidelity standards
Subtle pathologies can be invisible on displays that cannot render the full grayscale spectrum. This limitation can lead to missed diagnoses of conditions like faint nodules or micro-calcifications.
Medical-grade displays adhere to the DICOM 3.14 GSDF standard using high-bit-depth lookup tables, revealing faint pathologies that are lost on standard 8-bit consumer panels.
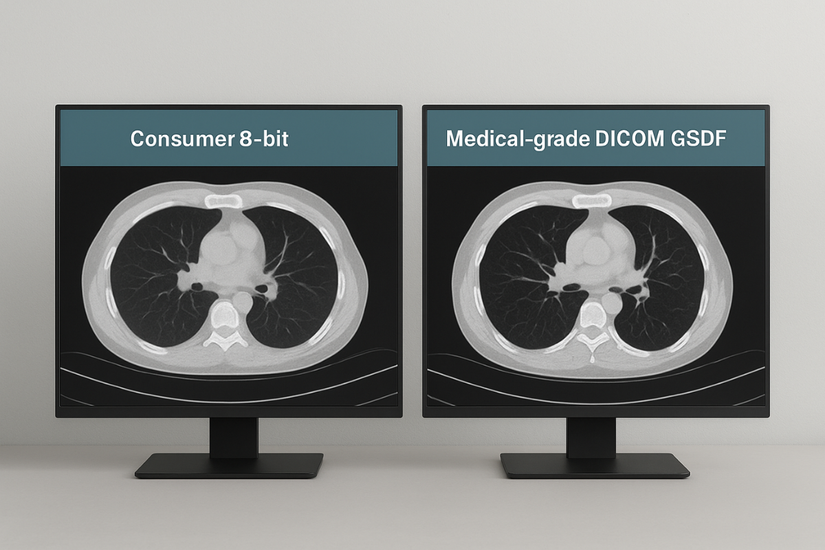
The cornerstone of diagnostic fidelity in medical imaging is the DICOM Part 3.14 Grayscale Standard Display Function (GSDF)10. This standard dictates a precise relationship between the digital value in an image file and the luminance level displayed on the screen, ensuring predictable and consistent grayscale perception. Medical-grade displays achieve this through the use of high-bit-depth lookup tables (LUTs)11, often 10-bit to 14-bit. This allows for up to 16,384 distinct shades of gray, a massive leap from the 256 shades available on a standard 8-bit consumer monitor. This vast dynamic range is what makes it possible to visualize extremely subtle findings, such as faint ground-glass opacities in a lung CT, tiny micro-calcifications on a mammogram, or small hemorrhages in a brain scan. Furthermore, many medical displays have built-in front sensors that continuously measure screen brightness and automatically adjust it to maintain perfect GSDF compliance over thousands of hours of use, preventing the performance drift that could otherwise mask critical diagnostic information.
Why not consumer screens?
Using off-the-shelf consumer monitors for telemedicine seems cost-effective but introduces unacceptable variability. Their inconsistent performance can lead to different clinical interpretations of the exact same image.
Consumer monitors lack the stabilized backlights, uniformity correction, and automated quality control of medical-grade displays, creating diagnostic variability that undermines the goal of telemedicine.
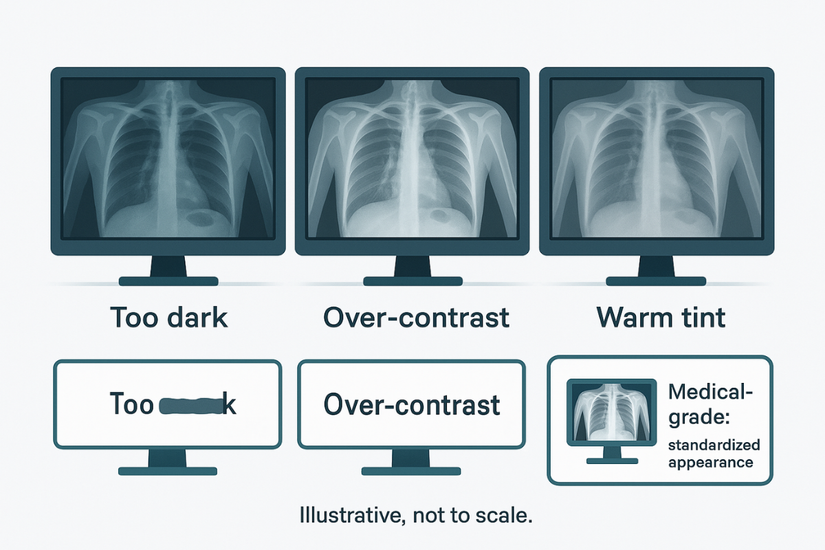
While tempting from a budget perspective, relying on consumer-grade monitors for clinical telemedicine applications is a critical error. These displays are built for a different purpose and lack the essential features required for diagnostic confidence. Their brightness, white point, and color settings vary dramatically from one unit to the next and can drift by more than 20% during warm-up alone. They also suffer from poor luminance uniformity, where the edges and corners of the screen can be significantly dimmer than the center, potentially hiding low-contrast lesions located in those areas. Most importantly, they have no mechanism for automated quality assurance or DICOM compliance12. In contrast, medical-grade displays are engineered to solve these problems. They feature stabilized backlights for constant luminance, apply digital uniformity correction at the factory, are calibrated to the DICOM GSDF standard, and include software for generating auditable quality assurance logs. This ensures that an image is rendered repeatably and reliably across different shifts, sites, and clinicians.
End-to-end sync across sites
Telemedicine collapses if the same image appears differently to the referring physician and the remote specialist. This "image drift" causes confusion, reduces diagnostic confidence, and delays patient care.
Achieving end-to-end synchronization requires standardizing on DICOM-calibrated medical-grade displays and using image-aware codecs, which ensures images remain identical from acquisition to final interpretation.
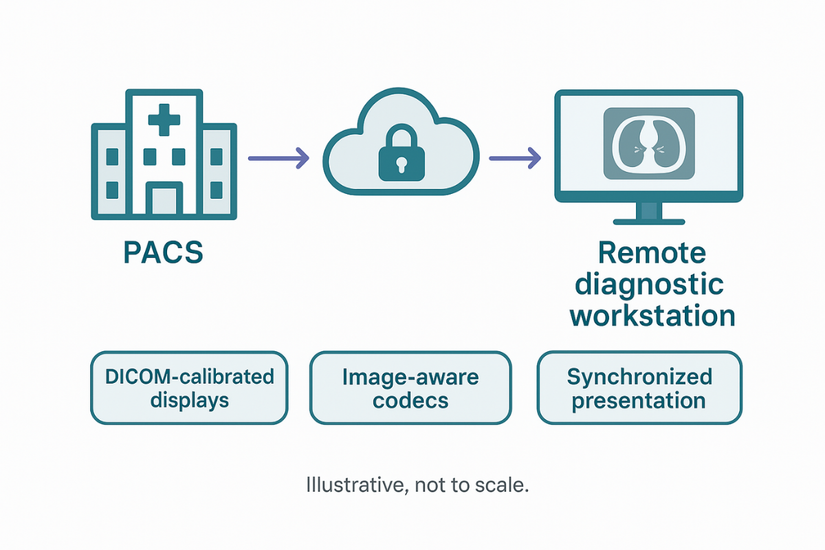
The fundamental promise of telemedicine is the seamless extension of expertise across distances. This promise is broken the moment the same image is perceived differently on two separate screens. Resolving this challenge requires a multi-layered, end-to-end approach to synchronization. The foundation is standardizing hardware, ensuring that both sending and receiving sites use medical-grade displays calibrated to the identical DICOM curve and white point. The second layer is the transmission pipeline. It is crucial to use codecs that are optimized for medical imaging and preserve fine textures and subtle grayscale data without introducing compression artifacts. The final layer is the user interface itself, where features like synchronized scrolling13 and presentation states ensure that when one clinician zooms in on an area of interest, the other clinician’s view follows precisely. When these elements are in place, the system fosters trust and efficiency. Clinical teams report a significant drop in equivocal or uncertain readings and an acceleration in confident decision-making.
Continuous QA & compliance
Without regular checks, display performance drifts over time, slowly degrading image quality. Manual calibration is time-consuming, disruptive, and often neglected in busy remote environments.
Medical-grade displays with embedded sensors and remote management software automate quality assurance, producing auditable logs that ensure continuous compliance with accreditation standards and maintain diagnostic confidence.
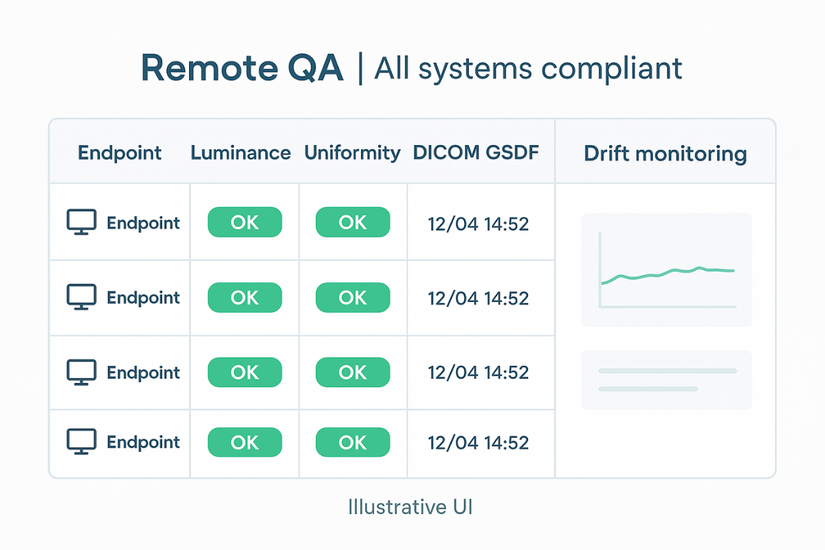
Accrediting bodies like The Joint Commission and the American College of Radiology mandate routine verification of diagnostic display performance. Managing this in a distributed telemedicine network with hundreds of remote workstations would be a logistical nightmare using manual methods. This is where the automation features of medical-grade displays become indispensable. Many models include a built-in front sensor that works with remote quality assurance (QA) software14. This system can be scheduled to run calibrations automatically during off-hours, measuring luminance, checking DICOM conformance, and logging the results without any user intervention. This creates a complete, auditable trail documenting each display’s performance over time, including the date, target luminance, and any deviations. This automated approach15 not only saves countless hours of manual work and minimizes clinical downtime but also guarantees that the entire fleet of displays remains compliant with regulatory requirements, thereby sustaining long-term diagnostic confidence across the organization.
Market momentum & demand
Healthcare systems face growing pressure from aging populations and the rise of chronic disease. They must find more efficient ways to deliver specialized care and conduct follow-up.
The global telemedicine market is projected to triple by 2032, fueled by demographic trends and the need for efficient chronic care. This growth creates sustained demand for medical-grade displays.
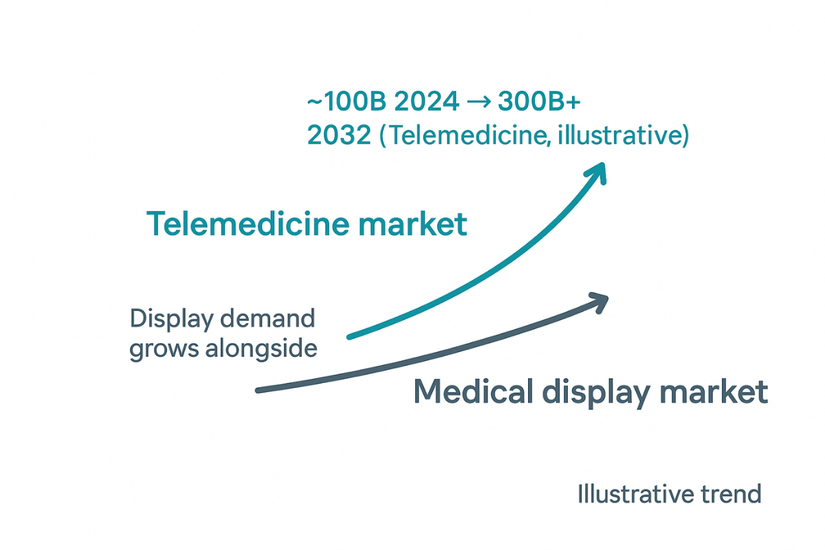
The growth trajectory for telemedicine16 is steep and sustained. The global market, valued at over $100 billion in 2024, is projected to exceed $300 billion by 2032, expanding at a compound annual growth rate (CAGR) of around 16-17%. The medical display market is growing in tandem, projected to increase from approximately $2.2 billion in 2022 to $3.6 billion by 2032. This momentum is driven by powerful, long-term trends. Aging populations and the increasing prevalence of chronic conditions necessitate more frequent follow-up and monitoring, much of which can be done remotely. The normalization of remote work has made teleradiology and other off-site clinical services a permanent fixture. The demand for 24/7 imaging coverage to support emergency departments and trauma centers further fuels the need for distributed reading networks. These factors create continuous and expanding demand for compliant, high-performance medical-grade displays across key service lines, including radiology, oncology, critical care, and perioperative medicine.
Deployment checklist & TCO
Deploying a fleet of remote diagnostic workstations without clear technical standards invites inconsistency. A poor initial investment leads to higher long-term costs from support issues and replacement cycles.
Prioritizing key specifications like DICOM compliance, high bit depth, and automated QA from the outset leads to fewer image-quality incidents and a lower total cost of ownership (TCO).
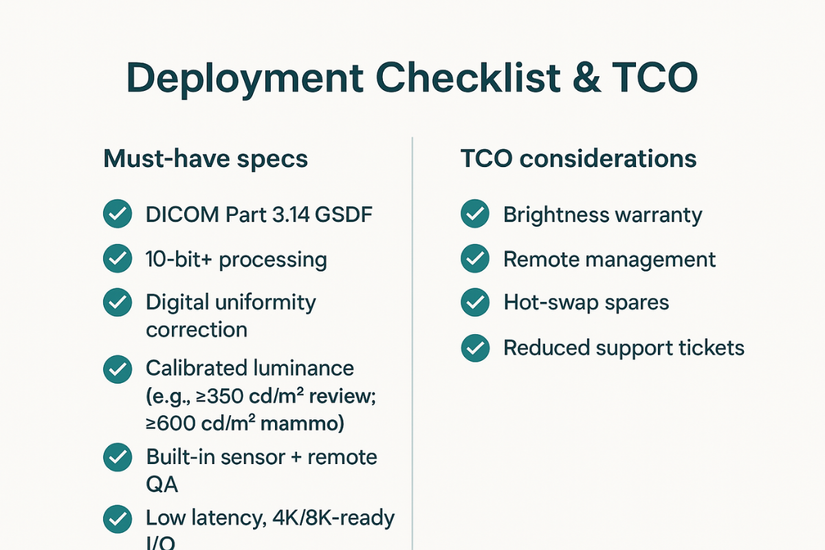
A successful and cost-effective telemedicine display deployment begins with a clear technical checklist. Prioritizing the right features ensures clinical efficacy and minimizes long-term expenses. Key specifications should include mandatory adherence to DICOM Part 3.1417, a minimum of 10-bit color/grayscale processing, and a calibrated luminance appropriate for the task (e.g., ≥350 cd/m² for clinical review, ≥600 cd/m² for mammography). Essential features also include digital uniformity correction, a built-in sensor for automated calibration, and remote QA management software. On the hardware side, low-latency processing and modern inputs (like DisplayPort or USB-C) capable of handling 4K or 8K signals are critical. When evaluating total cost of ownership (TCO)18, it is important to look beyond the initial purchase price to consider the manufacturer’s brightness warranty, the availability of hot-swap spare units, and the efficiency gains from reduced manual IT intervention. Healthcare organizations that standardize on these specifications report significantly fewer image-quality-related support tickets and a lower, more predictable TCO over the lifecycle of the equipment.
Documented clinical uplift
Investing in specialized technology requires proof of a tangible return. Without clear evidence of improved outcomes or efficiency, decision-makers are hesitant to approve the higher cost of medical-grade equipment.
Programs using medical-grade displays consistently report significant clinical gains, including ~40% faster radiology turnaround, higher productivity, and improved outcomes, validating the initial investment.
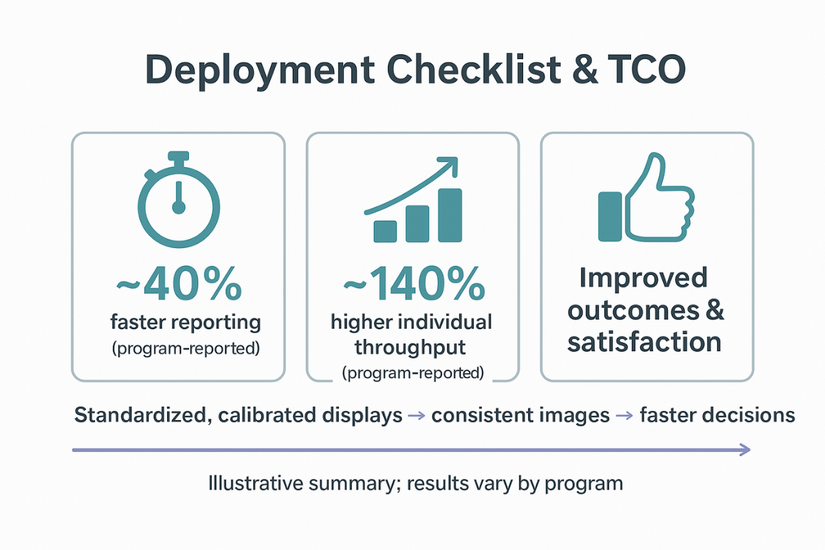
The evidence supporting the use of medical-grade displays in telemedicine is compelling and consistent across multiple clinical domains. The data reveals a clear pattern: trustworthy, identical images drive faster decisions and better outcomes. Teleradiology programs19 have documented up to a 40% reduction in final report turnaround times and an astonishing 140% increase in individual reader throughput after implementing standardized, calibrated workstations. In critical care, Tele-ICU programs have demonstrated that high-quality, reliable visualization contributes to fewer patient transfers and improved clinical outcomes. In collaborative medicine, clinicians report overwhelmingly high satisfaction with virtual MDT meetings that utilize synchronized, diagnostically accurate displays, citing more efficient and effective case discussions. This body of evidence provides a strong clinical and financial justification for the initial investment in medical-grade technology, proving that it is not a luxury but a foundational component of safe and effective telemedicine.
Conclusion
Medical-grade displays are essential for safe, effective, and efficient telemedicine, ensuring diagnostic confidence and fostering collaboration by delivering consistent, high-fidelity images across any distance.
-
Understanding medical-grade displays is crucial for ensuring accurate remote diagnostics and effective telemedicine practices. ↩
-
Exploring telemedicine applications can provide insights into how healthcare is evolving and improving patient care. ↩
-
Understanding GSDF is crucial for ensuring diagnostic accuracy in remote radiology, making this resource invaluable. ↩
-
Exploring the benefits of calibrated displays can enhance your knowledge of efficiency in remote radiology practices. ↩
-
Learn about the significance of factory calibration in ensuring true-to-life color accuracy, crucial for effective medical assessments.
patient and enhances the accuracy of documentation during the virtual visit. ↩ -
Explore how medical-grade displays enhance collaboration and ensure accurate image interpretation in virtual meetings. ↩
-
Learn about DICOM calibration’s role in maintaining image quality and consistency for better clinical outcomes. ↩
-
Learn about the significance of high bit depth in medical displays for accurate color reproduction and precision in surgical environments. ↩
-
Explore how Tele-ICU programs enhance patient care and improve outcomes in critical situations. ↩
-
Understanding GSDF is crucial for ensuring accurate medical imaging, making this resource invaluable for professionals in the field. ↩
-
Exploring LUTs will enhance your knowledge of how medical displays achieve superior image quality, essential for accurate diagnostics. ↩
-
Learn about DICOM compliance and its critical role in ensuring consistent and accurate medical imaging. ↩
-
Exploring synchronized scrolling can enhance your knowledge of effective telemedicine practices and improve clinician collaboration. ↩
-
This link will help you understand the critical role of QA software in maintaining display standards and regulatory compliance. ↩
-
Exploring this resource will provide insights into how automation enhances efficiency and compliance in telemedicine. ↩
-
Explore this link to understand the rapid advancements and future potential of telemedicine, a key player in modern healthcare. ↩
-
Understanding DICOM Part 3.14 is crucial for ensuring compliance and enhancing image quality in telemedicine. ↩
-
Exploring TCO helps organizations make informed decisions, ensuring long-term savings and efficiency in telemedicine deployments. ↩
-
Discover how Teleradiology programs can significantly reduce report turnaround times and enhance reader throughput in healthcare. ↩



