Grayscale drift makes the same CT/MR/DR look different across displays. This article shows why it happens and how to stop it fast with DICOM Part 14 (GSDF) calibration, CBS luminance stabilization, and ambient-light compensation—so lesion visibility stays reliable and your QA stays defensible.
When a radiologist says an image “looks different,” it is not a subjective complaint; it is a critical system failure. The ability to reliably compare a patient’s current scan with a prior study—often performed on a different machine and viewed on a different display—is the bedrock of modern radiology. Any deviation in how grayscale values are rendered breaks this fundamental chain of reproducibility. This guide explores the root causes of this “grayscale drift1,” its clinical and operational consequences, and the essential role of DICOM Part 14 (GSDF) calibration2 in establishing a standardized visual language. In short: we turn a variable perception problem into a measurable, controllable, solved data problem.
What “Grayscale Drift” Really Means—from Pixels to Perception
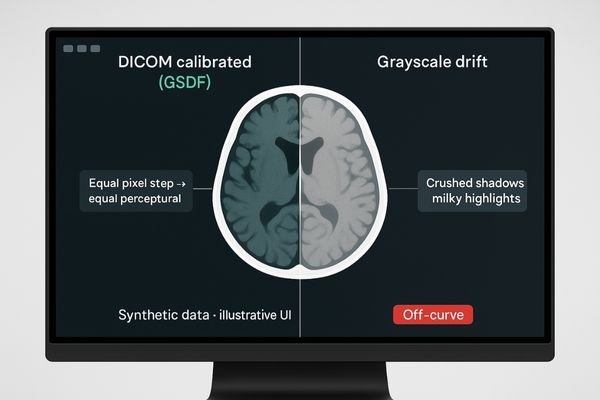
“Grayscale drift” is a systematic shift in a display’s dark-to-bright response. It causes crushed shadows and milky highlights, displacing lesion contrast and disrupting the perceptual consistency defined by DICOM Part 14.
An image file contains precise numbers, yet a display can render it in countless ways. That variability is not cosmetic—it is a break in the imaging chain.
Symptoms at a glance
- Crushed shadows: dark details disappear even at the same window/level.
- Milky highlights: bright structures lose separation and appear washed.
- Altered window/level feel: the tonal ladder no longer matches muscle memory.
- Cross-site mismatch: the same study conveys different cues in different rooms.
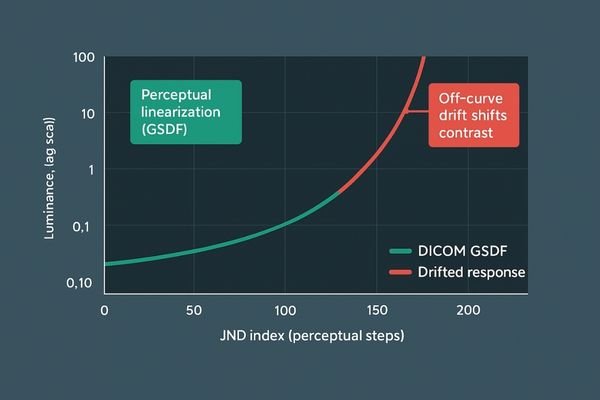
Why GSDF matters
DICOM Part 14 (GSDF)3 maps equal pixel steps to equal perceptual steps. When a monitor operates off-curve—or drifts over time—reading consistency4 collapses. Locking the pixel → luminance → perception chain to GSDF restores a shared visual language across devices and sites.
More Than a Tender Score: Clinical Detection, Collaboration, and Re-scan Ripple Effects
Clinically, drift obscures subtle findings, increases read times, and complicates consensus. Operationally, it drives tickets, re-scans, and compliance risk—a cascade of inefficiency.
When grayscale is inconsistent, uncertainty infects clinical judgment and operations alike.

Clinical impact
- Subtle-contrast findings at risk: tiny calcifications5, faint GGNs, isodense bleeds, mild enhancement.
- Longer time-to-read: more tweaking of window/level to compensate for non-standard response.
- Harder consensus: tumor boards see different cues on different displays.
- Follow-up distortion: small tonal shifts can mask real progression or regression.
Operational impact
- Recurring “looks different” tickets that consume IT and physics time.
- Training overhead as staff learn to work around inconsistent perception.
- Reading-room mismatches across sites, raising communication and coordination cost.
- Audit pressure when acceptance and constancy evidence is thin.
Where the Drift Starts: Panel Aging, Ambient Light, and Missing Part-14 QA
Drift originates from device aging, ambient light interference, and missing QA. Without measuring and correcting these factors, consistency will not last.
Grayscale inconsistency is predictable once you inspect device, environment, and process together.
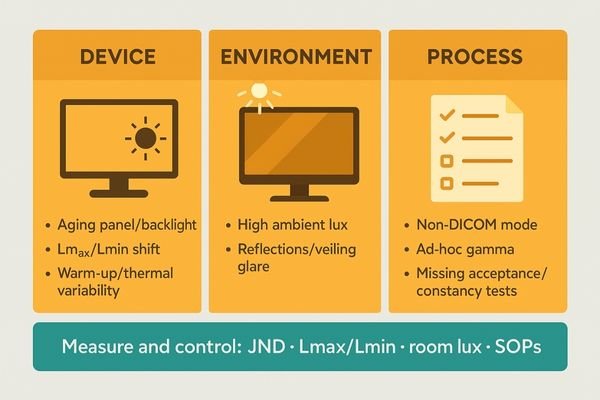
Three-layer model
1) Device — Backlight and panel aging shift Lmax/Lmin and gamma; warm-up and thermal swings add short-term instability.
2) Environment — Room lux, reflections, and veiling glare flatten at-site contrast, diluting the effective GSDF.
3) Process — Non-DICOM modes, ad-hoc gamma, and missing acceptance and constancy tests scatter parameters across a fleet.
Make it measurable
Use a data loop to track JNDs, Lmax/Lmin, contrast threshold, and room lux; encode warm-up, calibration, and spot checks into SOPs; control scaling and processing across the signal chain (GPU, cables, converters) to avoid non-linearities.
| Drift Factor | Source of Inconsistency | Mitigation Strategy6 |
|---|---|---|
| Device aging7 | Backlight and LCD degradation shift Lmax/Lmin and gamma. | Use displays with CBS luminance stabilization and auto DICOM (GSDF) calibration; 30-minute warm-up before QA. |
| Environment | Reflections and high ambient lux flatten perceived contrast. | Control reading-room lighting to 25–50 lux; reduce glare and veiling reflections; enable ambient-light compensation. |
| Process | Non-DICOM mode, ad-hoc gamma, missing acceptance and constancy tests. | Enforce Part-14 acceptance plus monthly or quarterly constancy tests; log JND, Lmax/Lmin, and room lux in SOP. |
Quick QA checklist: JND within spec · Lmax/Lmin documented · Room lux 25–50 · Warm-up complete · GSDF mode locked · Change log kept.
Lock the Ladder: Reshin’s GSDF + CBS Stack and Recommended Models
The stack combines GSDF auto-calibration, CBS luminance stabilization, and ambient-light compensation to lock consistency from both technical and workflow angles.
Fighting drift requires a proactive, automated system, not ad-hoc spot checks.
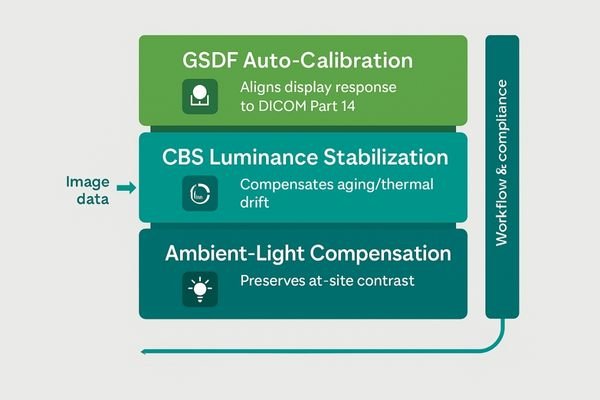
Technology stack
- GSDF auto-calibration8 — On-board sensing and curve correction keep response aligned with DICOM Part 14, reducing manual QA.
- CBS luminance stabilization — Compensates aging and thermal drift, holding Lmax/Lmin and target luminance within control bands.
- Ambient-light compensation9 — Adapts output to room lux to preserve at-site contrast.
- Workflow and compliance — Acceptance and constancy templates, automated logs, CE MDR documentation, and a 5-year warranty for predictable TCO.
Recommended diagnostic models (reading rooms)
| Model | Resolution | Key Functions | Typical Use |
|---|---|---|---|
| MD52G | 2048×2560 | Auto GSDF, CBS, ambient sensor | CT/MR-heavy primary reads, long-hour stability |
| MD46C | 2560×1440 | Auto GSDF, CBS, ambient sensor | DR/CT/PACS mixed workloads, balanced TCO |
| MD33G | 1536×2048 | Auto GSDF, CBS, ambient sensor | Compact diagnostic bays, secondary reads |
| MD32C | 1536×2048 | Auto GSDF, CBS, ambient sensor | Budget-sensitive rooms, standardized fleets |
| MD22CA | 1600×1200 | Auto GSDF, CBS, ambient sensor | General PACS viewing, training stations |
| MD26C | 1920×1200 | Auto GSDF, CBS, ambient sensor | Department rollouts needing consistent tone |
Standardizing a diagnostic fleet around GSDF, CBS, and ambient sensing unifies perception enterprise-wide: one curve, one look, one training footprint.
When Consistency Becomes ROI: Win Rate, Margin, and After-Sales Costs
Consistency is an operational asset: higher win rates with deliverable compliance and QA logs, protected margins with fewer re-reads and returns, and a predictable TCO from standard models and SOPs.
Standardizing on DICOM-compliant displays is not a sunk cost; inconsistency is.
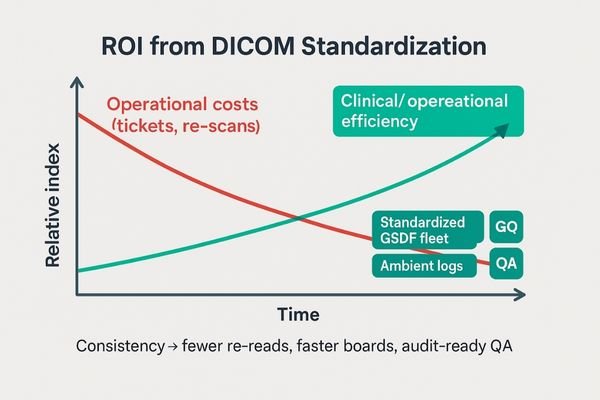
Procurement and compliance
- Tender strength: verifiable DICOM Part 14 compliance10 and log evidence accelerate acceptance.
- Audit-readiness: constancy records and ambient logs reduce review friction.
Clinical throughput
- Faster reads and boards: less time spent compensating for display behavior; smoother consensus.
- Fewer re-scans: stable perception prevents unnecessary repeats across sites.
IT and operations
- Fewer tickets: “looks different” incidents drop as GSDF stays locked.
- Lower training and spares: standardized fleet compresses learning curve and inventory.
Next Step: Standardize Your Grayscale — 【Get the Solution】
Take the next step toward eliminating grayscale drift. We will tailor a DICOM-compliant plan with GSDF auto-calibration, CBS luminance stabilization, and ambient-light compensation, plus acceptance and constancy templates and a diagnostic model shortlist for your reading rooms.
Moving from inconsistent grayscale to a standardized environment is a planned, evidence-driven process.
Get the Solution
Or email us: info@reshinmonitors.com
- Understanding grayscale drift is crucial for radiologists to ensure accurate image comparisons and maintain diagnostic integrity. ↩
- Exploring DICOM Part 14 calibration can enhance your knowledge of standardized imaging practices, vital for accurate diagnostics. ↩
- Understanding DICOM Part 14 (GSDF) is crucial for ensuring consistent image quality in medical imaging across different devices. ↩
- Exploring methods to maintain reading consistency can enhance diagnostic accuracy and improve patient outcomes. ↩
- Understanding tiny calcifications can enhance your diagnostic skills and improve patient outcomes. ↩
- Exploring mitigation strategies can enhance your knowledge on maintaining optimal display performance. ↩
- Understanding device aging can help you implement better maintenance strategies for display systems. ↩
- Understanding GSDF auto-calibration can enhance your knowledge of medical imaging technologies and their compliance with standards. ↩
- Exploring ambient-light compensation will provide insights into how displays maintain image quality in varying lighting conditions. ↩
- Understanding DICOM Part 14 compliance is crucial for ensuring interoperability and quality in medical imaging. ↩



