Hours into a Picture Archiving and Communication System (PACS) session, a radiologist feels the familiar ache behind their eyes. Grayscale details that were clear in the morning now seem to merge, forcing them to re-read images and question their own perception.
Long reading sessions amplify small visibility issues; high-brightness diagnostic monitors that sustain calibrated luminance and uniformity help preserve contrast perception in ambient light, reducing eye strain and rereads across PACS workflows.
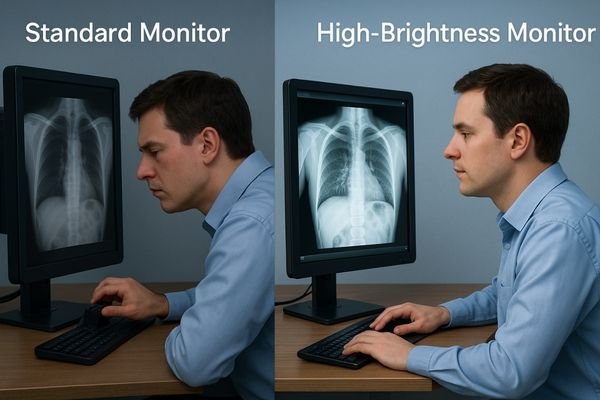
The work of a radiologist is one of intense and sustained visual focus. For hours on end, they perform complex visual searches, making thousands of micro-saccadic eye movements to detect subtle abnormalities within a sea of grayscale data. This high cognitive and perceptual load makes them uniquely susceptible to eye strain1—a direct threat to diagnostic accuracy and efficiency. One of the most significant environmental factors is the interaction between the diagnostic monitor and the ambient light of the reading room. When a monitor lacks sufficient brightness or fails to maintain calibrated luminance over time, the visual system must continually re-adapt; windows/levels are tweaked, posture tightens, and fatigue mounts. This article outlines practical, measurable steps to control luminance and reduce rereads.
Defining eye strain in radiology reading and display roles
Eye strain in radiology is not simply "tired eyes." It is a specific physiological response to a mismatch between the visual task, the display’s performance, and the viewing environment.
Eye strain is a physiological response to high cognitive load, sustained fixation, and luminance instability. High-brightness, DICOM-calibrated diagnostic monitors mitigate it by holding contrast in darker tones, resisting ambient washout, and stabilizing output over hours—so readers make fewer window/level changes and maintain confidence later in the shift.
Radiology reading is an exceptionally demanding visual task. It requires prolonged periods of intense focus, where the eyes constantly scan and fixate on regions of interest. This sustained effort, combined with the high cognitive load of interpreting complex images, creates ideal conditions for eye strain.
The Role of the Display
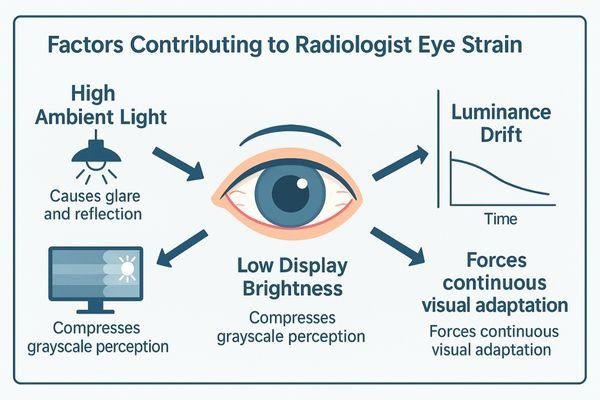
The diagnostic monitor sits at the center of this challenge. Eye strain arises when the monitor cannot present the image in a way that allows comfortable, efficient perception. This occurs when:
- Ambient light is high: Reflections and glare wash out the image, forcing the radiologist to squint to perceive contrast.
- Grayscale is indistinct: If luminance is too low, subtle differences between darker shades are compressed.
- Luminance drifts: Brightness fluctuates during long sessions, forcing continual re-adaptation.
High-brightness diagnostic monitors2 are designed to counteract these factors. By providing sufficient luminance headroom, they overcome ambient reflections while maintaining calibration to the Digital Imaging and Communications in Medicine (DICOM) Part 14 Grayscale Standard Display Function (GSDF) so every grayscale step remains perceptually distinct and stable over time.
Why insufficient luminance and drift degrade diagnostic perception
When a monitor’s light output is too low or unstable, it directly undermines a radiologist’s ability to see the information contained within the image.
Low or drifting luminance compresses dark grayscale tones, triggering constant window/level adjustments, re-scans, and posture strain. Ambient light compounds the effect by washing out subtle findings. High-brightness monitors with stabilization keep contrast response consistent across hours and sources, reducing rereads and interaction effort per study.
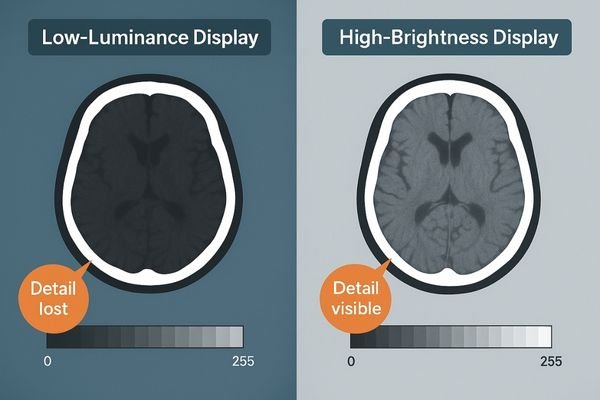
The diagnostic value of a medical image is encoded in its grayscale data3. Perception depends on accurate, consistent rendering. When peak luminance is insufficient—or drifts downward during a long session—the perceptual integrity of the image is compromised.
Compression of Grayscale Information
The most significant issue is the compression of mid-to-dark grayscale steps. On a dim monitor, subtle differences in tissue density appear as a single shade of dark gray. To compensate, a radiologist manually and frequently adjusts window/level, breaking concentration and adding time to each study. They may also lean in, squint, or re-scan regions of interest to confirm what they are seeing. High-brightness monitors with active stabilization keep the contrast response consistent for hours, preserving fine detail visibility and supporting comfortable adaptation.
Hidden costs of eye strain across quality, throughput, and safety
The impact of eye strain extends far beyond individual discomfort, creating tangible costs that affect the entire department’s performance.
Sustained eye strain increases reread rates, extends turnaround times, and elevates late-shift error risk. For leadership, that means unpredictable quality metrics, lower throughput, and governance drift—unless perception is stabilized with calibrated, high-brightness diagnostic monitors and room policies.
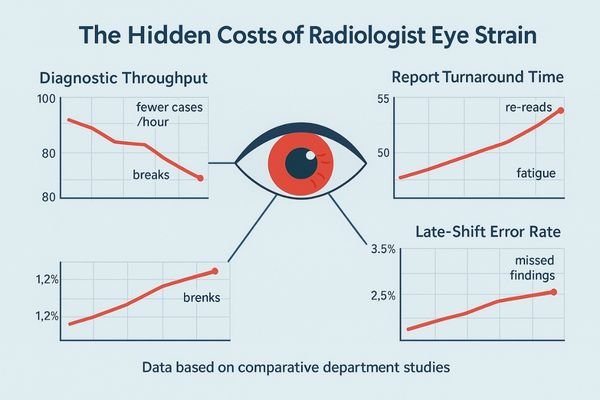
While often viewed as a personal comfort issue, chronic eye strain4 carries measurable costs for the healthcare organization.
Impact on Quality and Throughput
Productivity declines as visual fatigue grows. Frequent rereads and window/level changes extend study completion time, directly impacting report turnaround and throughput. The effect magnifies late in a shift, where perceptual fatigue can drive missed or misinterpreted findings. Refer to internal service logs and reading-room analytics (e.g., quarterly dashboards) to quantify patterns and track remediation.
Operational and Governance Costs
Eye strain fuels a cycle of inefficiency, including escalation calls to IT or clinical engineering about “inconsistent images.” The biggest leadership risk is loss of predictability: if perception varies with time of day, ambient light, or workstation, quality metrics and scheduling drift. Standardizing luminance and QA restores repeatability and resource control.
A practical luminance strategy for long, mixed-modality reading
A proactive strategy is required to move from fighting symptoms to solving root causes with a controlled, verifiable reading environment.
Combine room-level luminance targets, automatic monitor stabilization to compensate for drift, and clear policies on task lighting and glare control. Define measurable thresholds, log conformance, and verify during acceptance so the environment remains consistent through long sessions.
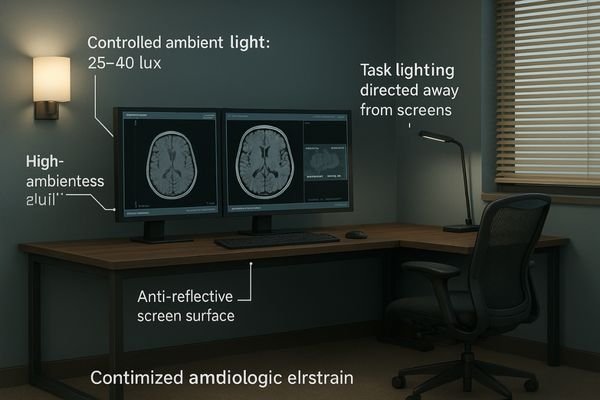
An effective strategy must address the entire reading environment, not the monitor in isolation. It starts with defining clear, room-level targets.
Define Targets and Automate Control
Establish a target peak luminance5 for all diagnostic monitors that provides explicit headroom above measured ambient light at the screen surface (lux). Pair targets with strict DICOM GSDF adherence to ensure perceptual linearity, and enforce them via built-in, continuous stabilization that compensates warm-up and aging. KPI suggestions: ambient lux logged quarterly; calibrated luminance documented with headroom; drift threshold and corrective action recorded in QA software; ≤60-second verified recovery to target after warm-up.
Control the Environment
Manage light with adjustable task lighting, blinds/shades, and workstation placement to minimize reflections. Publish a room-light policy defining acceptable lux ranges and glare-source mitigation for all reading rooms. Establish modality-specific window/level presets to reduce unnecessary manual adjustments and visual fatigue.
Selecting diagnostic monitors: brightness headroom, stability, and QA
The choice of diagnostic monitor is the most critical decision in implementing a luminance strategy.
Prioritize high-brightness panels for ambient resistance, fast warm-up with continuous stabilization, and comprehensive QA features such as uniformity correction and factory DICOM calibration reports. Require documented uniformity acceptance criteria and front-sensor/preset options validated at acceptance, plus reliable EDID behavior and dual-input layouts.
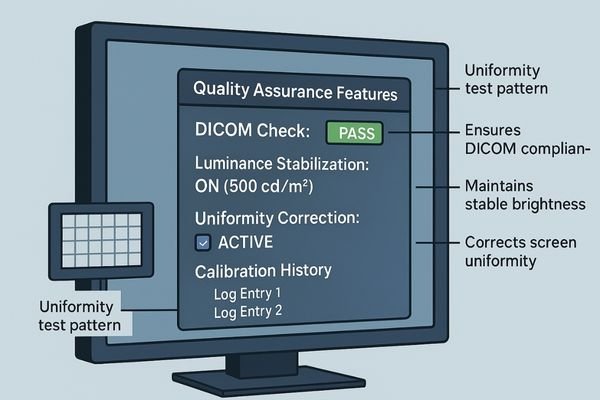
When selecting diagnostic monitors, focus on specifications that directly reduce eye strain over long sessions.
Core Technical Priorities
- Brightness headroom: Peak luminance significantly higher than the calibrated target to overcome ambient light and extend backlight life.
- Stability and warm-up: Continuous stabilization should be active and validated in acceptance tests to maintain consistent luminance hour after hour.
- Built-in quality assurance: Uniformity correction ensures even illumination; require detailed factory DICOM/GSDF reports and software hooks for in-field QA checks.
Recommended Diagnostic Monitors
| Model | Score | Suitability and Key Features for Reducing Eye Strain |
|---|---|---|
| MD33G | 86/100 | 3MP color for general PACS; strong brightness headroom and stabilization for mixed CT/MR. |
| MD52G | 90/100 | 5MP grayscale for high-contrast tasks; calibrated luminance protects subtle findings. |
| MD120C | 92/100 | Unified 12MP reading; superior brightness and uniformity reduce window/level fatigue. |
Business value: predictable quality and lower total ownership cost
Investing in stabilized, high-brightness diagnostic monitors is an investment in the department’s core function, delivering returns through efficiency, quality, and asset longevity.
Stable perception reduces rereads and improves throughput, lowering staffing costs. Standardized calibration and fewer manual tweaks cut QA time, while brightness headroom extends usable life. Track reread rate, average study turnaround, and after-hours staffing variance before/after deployment to quantify ROI.
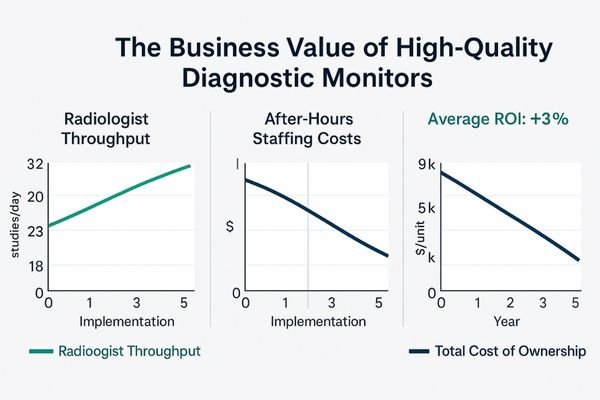
The business case is straightforward. When radiologists maintain stable perception across shifts, departmental efficiency improves. Fewer rereads and faster interpretations boost throughput and reduce reliance on after-hours or locum staffing. Standardizing on calibrated, stabilized monitors lowers ownership costs by reducing manual QA and troubleshooting. Starting with ample brightness headroom delays replacement driven by dim screens or discomfort, extending fleet life. This content addresses display selection and QA processes and does not constitute medical advice.
FAQ for leadership: policy, targets, and room conditions
What peak luminance should we target for our reading rooms?
Set a calibrated target based on measured ambient light at the screen surface, with comfortable headroom. Confirm choices with DICOM GSDF conformance reports and reader feedback, and verify stabilization logs after targets are applied.
How do we maintain this target luminance over the monitor’s life?
Automate maintenance. Procure monitors with built-in stabilization and schedule software-driven QA checks that log drift and uniformity over time; lock settings via departmental policy and verify during quarterly QA.
Will higher brightness just add more glare and eye strain?
Not when implemented as part of a complete strategy. Brightness headroom should be paired with defined room-light ranges and anti-reflective surfaces to maintain consistent contrast perception without over-illumination.
Conclusion
High-brightness diagnostic monitors that maintain calibrated luminance, uniformity, and GSDF compliance are essential tools for reducing eye strain and stabilizing throughput in long-session reading environments. To request a luminance policy template and an acceptance QA checklist, contact info@reshinmonitors.com.
-
Understanding eye strain is crucial for radiologists to enhance their diagnostic accuracy and maintain eye health. ↩
-
Explore how high-brightness diagnostic monitors enhance image clarity and reduce eye strain for radiologists. ↩
-
Understanding grayscale data is crucial for improving diagnostic accuracy in medical imaging. ↩
-
Understanding the impact of chronic eye strain on productivity can help organizations implement better practices and improve overall efficiency. ↩
-
Understanding target peak luminance is crucial for optimizing monitor performance and ensuring accurate diagnostics. ↩



