During a critical remote consult, a surgeon describes a subtle erythema that the consulting specialist cannot see on their screen. This disconnect erodes confidence and delays the decision-making process.
Remote consults fail when displays render different hues and contrast. Standardizing on ITU-R BT.709 (Rec.709) with a D65 white point and BT.1886 gamma for color, and on the Digital Imaging and Communications in Medicine (DICOM) Part 14 Grayscale Standard Display Function (GSDF) for grayscale—then enforcing calibration and validating encoder behavior—restores a shared visual truth across sites.

Effective remote consultation, whether for live surgery or a complex radiology review, is built on the foundation of a shared visual truth. When clinicians in different locations discuss an image, they must be confident they are all seeing the same colors, the same contrast, and the same subtle details. Too often, this foundation crumbles due to technical inconsistencies1. Variations in display technology, color standards, calibration, and even the streaming codecs used to transmit the video create a scenario where each participant sees a slightly different version of reality. This isn’t a minor inconvenience; it is a fundamental barrier to effective communication that introduces ambiguity, causes delays, and can ultimately impact clinical outcomes. Establishing a robust color governance strategy is no longer a luxury but a core requirement for any organization that relies on remote visual collaboration.
Why color mismatches derail remote surgical and radiology consults
Clinical language is precise, but it fails when the visual evidence is inconsistent. A description of "pale" or "inflamed" becomes meaningless if each screen tells a different story.
When displays are not calibrated to a common target, inconsistent rendering of skin tones and lesion contrast makes clinical language ambiguous, leading to skepticism, repeat explanations, and diagnostic delays; track cross-site color delta (e.g., average ΔE2000 within tolerance) and luminance drift logs, and audit encoder profiles per site to keep variance governed.
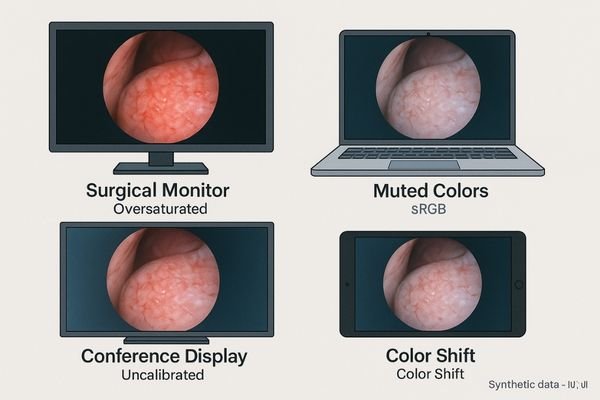
Remote consultations are derailed by a thousand tiny cuts of visual inconsistency2. The entire process hinges on the assumption that when one clinician describes a visual finding, the other can see it with the same fidelity. Color mismatches shatter this assumption. When the consulting surgeon’s high-end surgical display, calibrated to Rec.709, shows vivid red mucosal tissue, the remote expert might see a muted, slightly orange version on their standard RGB (sRGB) laptop display. The language used to describe the finding—"subtle erythema"—becomes subjective and open to interpretation. This forces a cycle of inefficiency. The presenter must spend extra time describing what they see, often resorting to clumsy workarounds like circling areas and taking screenshots. The remote consultant, unable to trust the color fidelity of the image, may become hesitant or overly conservative in their recommendations. This fundamental breakdown in shared visual understanding slows the pace of the consultation, erodes trust between participants, and introduces a dangerous level of ambiguity into the clinical decision-making process.
Root causes across color standards, devices, and streaming paths
Color differences are not random; they are the predictable result of a fragmented technology ecosystem where every component can alter the final image.
Mismatched standards (sRGB vs. Rec.709), uncalibrated white points, inconsistent gamma curves, and encoder-induced chroma subsampling are primary root causes of color drift in remote consults; manage them by defining targets, logging ΔE and luminance variance, and auditing bandwidth/codec settings on each site.
The journey of an image from the operating room to a remote consultant is fraught with potential points of color corruption. The issues stem from a lack of end-to-end standardization across three key domains.
Standards and Devices
Different devices are built to different standards. An endoscopy camera outputs a Rec.709 video signal, a typical office laptop uses an sRGB color space, and a PACS workstation is calibrated to the DICOM grayscale standard. Each of these has a different gamut, gamma curve, and white point. Without rigorous color management3, the image will look different on each device. Furthermore, panel aging causes even identical displays to drift apart in color and brightness over time if they are not recalibrated. sRGB and Rec.709 share primaries and D65, but system gamma handling differs; unmanaged OS/app color management often treats them interchangeably, creating perceptual mismatches.
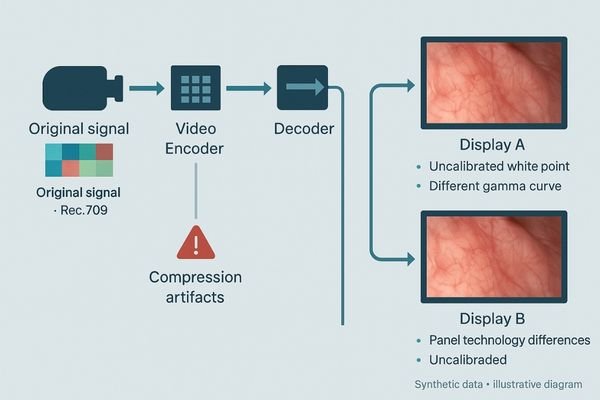
The Streaming Path
The streaming technology itself introduces another layer of variables. Video encoders often use chroma subsampling (e.g., 4:2:0) to save bandwidth, which can reduce color resolution. They may also perform gamut clipping or dynamic range conversions (full vs. limited) that alter the image. Even the adapters and scalers used to connect devices can silently transform the color space without the user’s knowledge, creating an unpredictable and unreliable imaging chain. Validate 4:2:2 vs. 4:2:0 chroma, prefer a 10-bit pipeline where feasible, enforce Rec.709 matrix coefficients and correct limited/full range mapping, and disable dynamic tone/contrast mapping during consults.
Clinical, operational, and compliance risks of color drift
When clinicians cannot trust the color they see, the consequences ripple outward, affecting patient safety, operational efficiency, and institutional risk.
Misaligned color confuses symptom description, slows case decisions, and increases medicolegal exposure; operationally, it drives up support costs and erodes trust in remote workflow infrastructure—set targets and track time-to-decision and color-related ticket rates to verify improvement.
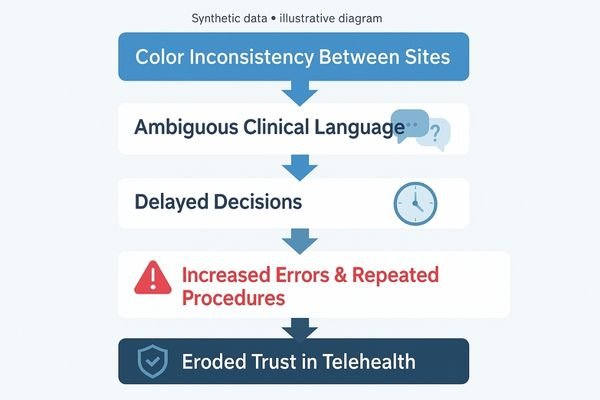
The risks associated with unmanaged color variation in a clinical setting are significant and multifaceted.
Clinical and Compliance Risks
Clinically, the most immediate risk is miscommunication. If a remote pathologist cannot accurately perceive the subtle difference in staining that indicates malignancy, a critical diagnosis could be delayed or missed. This forces clinicians to make more conservative decisions or trigger unnecessary in-person escalations, defeating the purpose of the remote consultation. This ambiguity also creates a compliance and medicolegal risk. If the color in a captured image used for documentation does not match what was seen during the live procedure and a poor outcome occurs, it can be difficult to defend the clinical record.
Operational Risks
Operationally, chronic color issues are a major drain on resources. They lead to a constant stream of IT support tickets and vendor service calls as frustrated clinicians try to troubleshoot the problem. Over time, this erodes the staff’s confidence and trust in the telehealth and remote consultation4 platforms, leading to low adoption rates for new and valuable workflows. For leadership, this creates a major predictability problem, undermining efforts to standardize care and govern quality across multiple sites. Define a color-governance service-level agreement (e.g., maximum ticket resolution time and quarterly pass-rate targets) to rebuild confidence.
A pragmatic color-governance strategy for remote consults
The solution is not to buy more adapters, but to create a disciplined, end-to-end strategy that enforces a single standard of visual truth.
Standardize on scene-appropriate targets like Rec.709, lock them with hardware calibration, verify encoder settings, and implement a lightweight, routine QA cadence to catch and correct drift early; document acceptance metrics (e.g., ΔE thresholds, luminance headroom) and keep a shared audit log across sites.

Creating a reliable remote consultation environment requires a deliberate color governance strategy. This strategy moves from reactive troubleshooting to proactive management of the entire imaging chain.
- Standardize on Targets: Define a single, appropriate standard for each use case. For color video sources like endoscopy, use Rec.709 with a D65 white point and BT.1886 gamma; for radiology images, use DICOM Part 14 GSDF. These targets are enforced under policy and audited across endpoints.
- Calibrate and Lock: Enforce standards through hardware Look-Up Table (LUT) calibration on every display so corrections are independent of OS/app behavior. Calibrated profiles should be versioned, centrally distributed, and locked to prevent accidental changes.
- Verify the Path: Audit video encoders/streaming apps to ensure no unwanted color-space or range conversions. Use common test charts (e.g., ColorChecker/SMPTE) for cross-site acceptance and record pass/fail to a shared log.
- Implement Routine QA: Build a quarterly QA cadence (or upon panel/firmware change) to measure and log ΔE and luminance variance against thresholds, allowing correction before clinical impact.
Display selection principles: headroom, presets, and integration
The display is the final endpoint in the imaging chain. Its native capabilities determine whether a color governance strategy is practical or even possible.
Choose displays with brightness headroom, stable factory presets for Rec.709 and DICOM, hardware calibration hooks, uniformity correction, and deterministic EDID behavior to ensure consistent, predictable performance; include acceptance criteria for uniformity and cross-site preset matching.

The success of any color governance strategy depends on the capabilities of the displays at each endpoint. When selecting displays for consultation environments, several principles are key. The display must have sufficient luminance headroom to overcome ambient light in different reading environments without washing out colors. It must have stable, accurate, and easily selectable factory presets for key standards like Rec.709, sRGB, and DICOM. Crucially, it must support hardware calibration5 via a direct connection to a colorimeter and compatible software, allowing for true LUT-level adjustments. Features like digital uniformity correction are essential for ensuring that color is consistent not just between displays, but across the surface of a single screen. From an integration perspective, the display must provide deterministic EDID behavior so that sources always connect reliably, and it should offer dual inputs for redundancy or for easy comparison of two sources. Require control of HDMI/DP InfoFrames to force Rec.709 signaling and correct limited/full range mapping across adapters/scalers. The value of a display increases significantly when a vendor can demonstrate and witness its proven interoperability with your specific encoders and conferencing applications, and before PO confirm factory color reports, lockable white point/gamma presets, 3D-LUT workflow, and the quarterly QA cadence.
Recommended Displays for Color Governance
| Model | Score | Suitability and Key Features for Color Governance |
|---|---|---|
| MD33G | 88/100 | 3MP color; accurate Rec.709/DICOM presets for cross-site consults. |
| MD32C | 86/100 | 32" color; hardware calibration hooks for shared reviews. |
| MS321PB | 84/100 | 32" 4K; Rec.709/BT.2020 presets align OR sources to consults. |
Business value: fewer escalations and predictable remote workflows
A well-implemented color governance strategy is not just a technical improvement; it is an investment that delivers tangible business returns.
Color governance reduces time wasted in debates, cuts support escalations, and shortens decision cycles; track time-per-consult, color-related ticket count, and post-install decision latency across sites to quantify ROI.
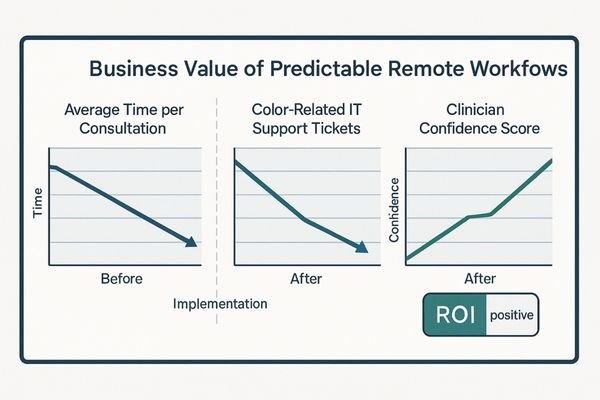
The business value of achieving color consistency across a remote consultation network is clear and measurable. The most immediate return is in operational efficiency. When all participants see the same image, the time lost to clarifying visual discrepancies, debating color interpretation, and sharing screenshots disappears. This shortens the time required for each consult and accelerates clinical decision-making. This efficiency gain directly translates to lower costs. The number of IT and vendor support calls related to "bad color" plummets, freeing up technical resources and reducing service expenditures. Training on remote workflows becomes simpler and more effective when the visual experience is consistent and predictable. Over the long term, this predictability builds clinician trust and drives adoption of telehealth initiatives. It also extends the useful life of a display fleet by ensuring assets can be maintained to a specific performance target, reducing surprise-driven capital expenses and lowering the total cost of ownership. This article addresses display/stream governance and QA processes and does not constitute medical advice.
FAQ for leadership: standards, HDR mixing, and calibration cadence
What standard should we use for color video consultations?
For all standard HD and 4K color video sources like endoscopy and conferencing, the organization should standardize on Rec.709 with a D65 white point and BT.1886 gamma. Grayscale radiology images should remain on the DICOM GSDF standard.
How do we handle new HDR screens in our remote workflows?
Mixing HDR and standard dynamic range (SDR) displays in a single consultation is a major source of inconsistency. Unless all endpoints are fully HDR-capable and calibrated to a common HDR target, disable automatic tone mapping and configure the entire chain to operate in matched, calibrated SDR (Rec.709). Enable HDR only when all endpoints are HDR-calibrated and the encoder preserves 10-bit depth and Rec.2020 signaling end-to-end.
Do our network video encoders really change the color?
Yes, they can significantly alter the appearance. Most encoders use 4:2:0 chroma subsampling to reduce bandwidth, which lowers color detail. They can also incorrectly handle conversions between full and limited video range. Validate encoder profiles, log profile versions and changes, and re-validate after firmware updates.
How often do we really need to calibrate these displays?
A full hardware calibration should be performed as a baseline at installation. After that, a lightweight QA check should be conducted on a quarterly basis or any time there is a major change, such as a panel replacement or a significant firmware update. This cadence ensures that drift is caught and corrected before it can impact clinical work.
Conclusion: align standards to restore a shared visual truth
By aligning standards, presets, room light, and encoder behavior, organizations can eliminate visual ambiguity and restore a shared truth for more effective remote consultation. To request a cross-site color governance checklist and acceptance templates, contact info@reshinmonitors.com.
-
Exploring the impact of technical inconsistencies can help improve remote consultation practices and enhance communication among clinicians. ↩
-
Understanding visual inconsistency can help improve remote consultations and enhance communication between clinicians. ↩
-
Understanding color management is crucial for ensuring accurate image representation across different devices, enhancing diagnostic accuracy. ↩
-
Exploring this topic can reveal insights into improving telehealth practices and ensuring better patient care ↩
-
Exploring hardware calibration can enhance your knowledge of achieving precise color accuracy in displays. ↩



