Juggling multiple displays in a cramped endoscopy suite creates clutter and divides clinical focus. Trying to consolidate sources onto one screen without a clear strategy risks confusion and errors.
Route with purpose and display with discipline: use 12G-SDI for locked 4K60 runs, DP for low-latency near-field, and reserve HDMI for utility. Pick fixed templates—PIP for reference, PBP for co-primary, quad for team awareness—then size panes to legibility thresholds and label them. Zero-drop switching and verified latency turn multiview layouts into safe, repeatable OR practice.
In modern endoscopy, the ability to view multiple video sources on a single screen is not a luxury; it is a clinical necessity. However, simply cramming more windows onto a display is a recipe for disaster. Effective multiview implementation1 is a discipline that combines robust signal routing2, ergonomic layout design, and rigorous technical validation. A successful system presents information intuitively, reduces cognitive load, and enhances team situational awareness. This guide details a practical methodology for designing and deploying multiview systems that are safe, reliable, and purpose-built for the demands of the endoscopy suite.
Choosing PIP vs PBP vs Quad: one-look decision rules
Without clear guidelines, clinicians may improvise screen layouts mid-procedure. This improvisation under pressure can lead to confusion, wasting precious time and increasing the risk of misinterpretation.
Assign the endoscopic feed dominance unless safety data must be persistently readable. Use PIP for consultative feeds, PBP for co-primary sources, and a fixed quad layout for team awareness.
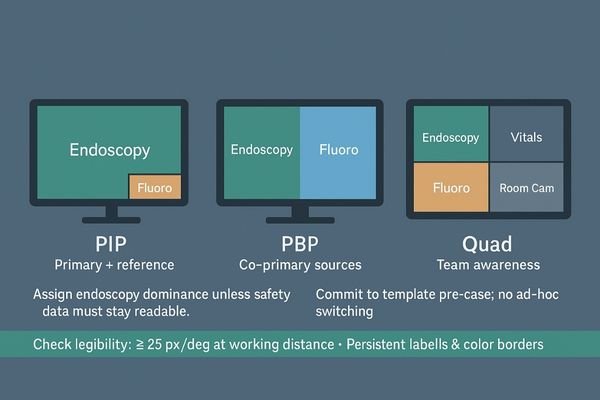
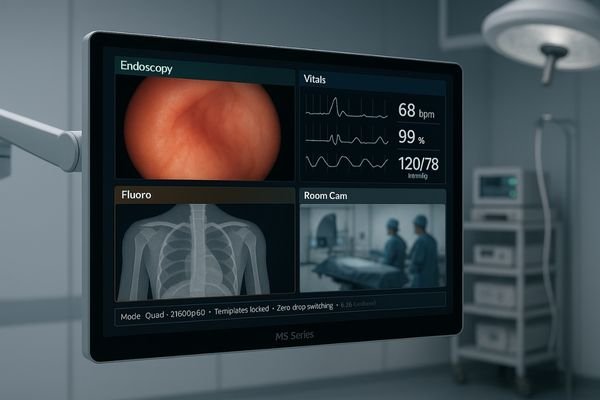
The choice between Picture-in-Picture (PIP)3, Picture-by-Picture (PBP), and a quad-view layout should follow a brutally practical set of rules based on the clinical priority of the information. The primary endoscopic feed must always have visual dominance unless a secondary source, like fluoroscopy or critical patient vitals, requires persistent, unambiguous legibility for safety. My decision framework is simple: if the secondary feed is purely for reference or consultation (e.g., a C-arm image), use a small PIP window that does not obstruct the main view. If two sources are co-primary and require simultaneous, focused attention (e.g., endoscopy and live ultrasound), a side-by-side PBP layout is appropriate. A multi-input monitor4 like the MS321PB allows for these flexible configurations. For cases where overall team situational awareness is paramount, a fixed quad-view template with clearly defined sources is the safest option. The most important discipline is to commit to the correct layout before the case begins, eliminating the need to make these decisions under stress.
| Layout | Primary Use Case | Example Sources |
|---|---|---|
| PIP | Primary view with a secondary reference | Endo (main) + Fluoro still (PIP) |
| PBP | Two co-primary, equally important views | Endo + Live Ultrasound |
| Quad | Full team situational awareness | Endo + Vitals + Anesthesia + Room Camera |
Signal routing that never flinches: 12G-SDI long runs, DP near-field, HDMI utility
An unstable video signal can cause screen blackouts or dropped frames at critical moments. A system built on unreliable, consumer-grade connections is a major liability in any surgical environment.
Build the video backbone on 12G-SDI for deterministic long runs. Use DisplayPort for short, low-latency hops to near-field displays, and treat HDMI as a utility input, not a primary transport.
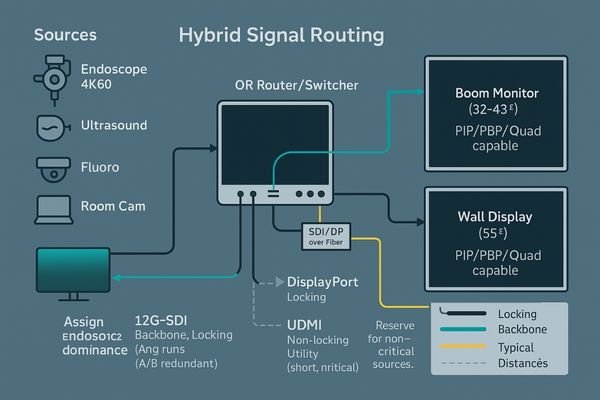
A multi-source display system is only as reliable as the signal paths that feed it. The success or failure of an entire OR integration hinges on routing. For delivering locked-in, uncompressed 4K60 video over the long distances required to cross ceilings and booms, 12G-SDI5 provides the most deterministic and mechanically secure performance. Its locking BNC connectors are a non-negotiable feature in an environment with vibration and movement. DisplayPort6 serves a different but equally important role as the ideal interface for short, near-field hops where minimizing latency is the top priority—for example, connecting a video source on a cart directly to its monitor. HDMI should be relegated to a utility input for non-critical sources like a PACS viewer or a laptop, as its connectors are not locking and its signal integrity is less robust over distance. Designing the system with A/B redundant paths and ensuring every cable is physically labeled is crucial. A large-format wall display like the MS550P, with its array of professional inputs, anchors this type of robust, hybrid routing scheme.
Layout that serves the case: source priority, pane sizing, and fixed labels
A poorly designed multiview layout can be worse than no multiview at all. If critical information is too small or placed illogically, it increases cognitive load and heightens the risk of errors.
A good layout honors clinical priorities. Size the primary pane for optimal legibility, fix the positions of secondary sources, and use persistent color-coding and labels to reduce cognitive strain.
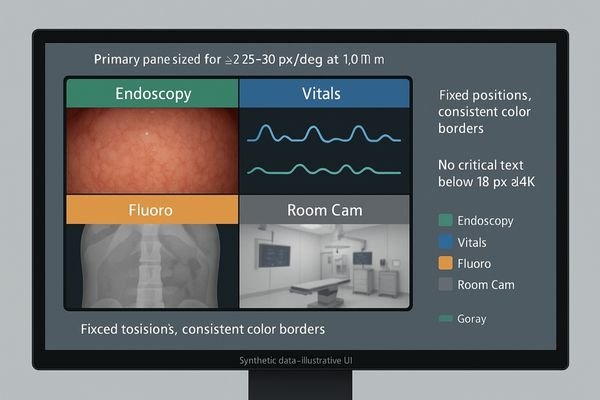
Effective multiview design is not about cramming as many panes as possible onto a screen; it is about presenting information in a way that respects clinical priorities. The process should begin by sizing the primary endoscopic pane to meet the standard of angular legibility7—it must subtend enough of the visual field to ensure at least 25 pixels per degree at the surgeon’s typical viewing distance. Once the primary pane is sized, the remaining screen real estate can be allocated to secondary sources like vitals or reference images, with hard minimums for size and resolution to ensure they remain readable. I strongly advocate for a standardized visual language8, using persistent color-coded overlays or borders for different source types (e.g., green for endoscopy, blue for vitals). This creates instant recognition. A 43-inch monitor like the MS430PC offers ample screen space to create these logical layouts without compromising the size of any single pane. In high-stress situations when staff are tired, fixed templates with clear labels dramatically reduce the hunt-and-seek errors that can occur with fully flexible matrix systems.
Sync, latency, and scaling: the hidden killers of multiview
The most dangerous problems in a multiview system are often invisible. Unsynchronized sources, poor image scaling, and added latency can subtly degrade performance and even compromise surgical precision.
Unsynced sources, poor scalers, and excess latency can ruin a multiview system. Demand zero-drop switching, verify low latency with real sources, and ensure the display’s scaler preserves critical line detail.
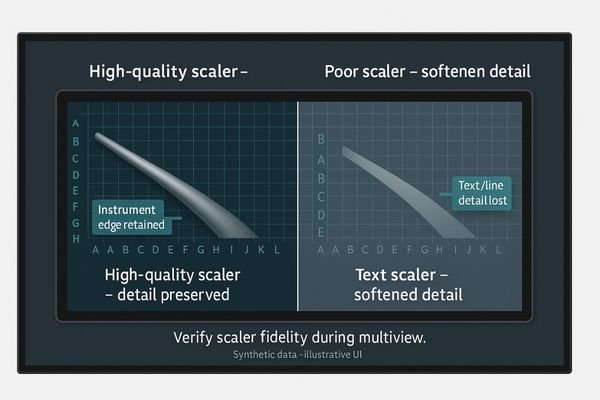
What often undermines multiview performance9 are the factors you cannot easily see. When video sources are not synchronized, switching between them or combining them on screen can trigger frame drops or visual tearing. The image scaler within the display is another critical component; a low-quality scaler will soften or smear fine details, like the edges of a surgical instrument or subtle tissue textures, when resizing a source to fit into a smaller pane. Finally, the processing required for multiview can add latency. Even a few extra frames of delay are enough to disrupt a surgeon’s sensitive hand-eye coordination. It is essential to stress-test the system with a 10-to-15-minute script of rapid source switching to ensure zero frame drops. Furthermore, glass-to-glass latency10 must be measured with actual clinical sources, not just static test patterns. A 4K monitor such as the MS275PA, designed for surgical use, incorporates high-quality processing to handle these challenges. If the performance is not consistent and repeatable, the system is not ready for clinical use.
Proving it works: acceptance tests, stress scripts, and failover drills
A system that works in a lab but fails under real-world pressure is a liability. Without a formal acceptance process, there is no guarantee that the system will perform reliably when it matters most.
Formal acceptance requires documented proof. This includes a stress-test report, latency measurements, and a clear, one-page failover drill that every member of the clinical team can execute.

A successful multiview deployment concludes with a rigorous acceptance and validation process11. This means documenting the complete "recipe" for the installation, including room-specific layouts, verified minimum pane sizes for legibility, and a full check of both primary (A) and redundant (B) signal paths. The process must be formalized with a pass/fail stress script that simulates a complex case, and the results must be signed off. A crucial and often overlooked component is the failover drill12. A simple, laminated, one-page guide should be created that clearly explains who does what, and in what order, if a primary source or display fails. This documentation ensures that any member of the team can respond correctly in an emergency without having to guess. This disciplined approach to validation,ensures that reliability is built-in and verifiable, not just assumed. The system is only truly "accepted" when it has been proven to be resilient.
Optics and hygiene in the OR: AR glass, bonded fronts, and wipe-clean design
Even a perfect video signal can be compromised by poor display optics. Glare, reflections, and surface contamination are the physical enemies of image contrast and clarity in the bright environment of an OR.
Superior optics and hygiene are non-negotiable. An anti-reflection, optically bonded front surface maximizes contrast, while a sealed, wipe-clean design is essential for infection control and long-term reliability.

The final link in the quality chain is the physical surface of the display itself. In the brightly lit environment of an endoscopy suite, reflections and glare can wash out an image, destroying contrast and hiding subtle details. This is why professional surgical displays use anti-reflection (AR) coated protective glass13. This glass should be optically bonded directly to the LCD panel underneath, which eliminates the internal air gap that causes reflections and traps condensation. This design choice maximizes image clarity and perceived contrast. Hygiene is equally important. The monitor must have a sealed, flat front surface14 that is easy to wipe down and disinfect without fear of fluids seeping into the electronics. A monitor like the MS322PB is engineered with these critical features. In endoscopy, the fight for clinical clarity and the fight for cleanliness are one and the same; a display that compromises on either is not fit for purpose.
Conclusion
Resist the "anything-anywhere" matrix fantasy; instead, standardize on a few fixed multiview templates that match your primary procedures and train your team to use them with muscle memory. 🖥️
👉 For advanced multiview surgical display solutions and expert guidance, contact martin@reshinmonitors.com.
-
Explore this link to understand how effective multiview implementation can enhance clinical outcomes and team efficiency. ↩
-
Learn about signal routing to grasp its critical role in ensuring reliable and high-quality video feeds in endoscopy. ↩
-
Explore the benefits of PIP in surgery to enhance your understanding of its practical applications and improve patient safety. ↩
-
Learn about essential features of multi-input monitors to make informed decisions for surgical environments and improve efficiency. ↩
-
Explore the benefits of 12G-SDI for reliable video transmission, especially in environments with vibration and movement. ↩
-
Learn how DisplayPort can enhance your video setup by minimizing latency for near-field connections. ↩
-
Understanding angular legibility is crucial for creating effective visual layouts that enhance readability and usability. ↩
-
Exploring standardized visual language can help you create intuitive designs that enhance user experience and recognition. ↩
-
Understanding the factors affecting multiview performance can help optimize video systems for better results. ↩
-
Exploring this topic will provide insights into ensuring optimal performance in surgical environments. ↩
-
Understanding this process is key to ensuring successful multiview deployments and system reliability. ↩
-
Exploring this topic will highlight the significance of preparedness in emergency situations, ensuring team readiness. ↩
-
Explore how AR coated glass enhances image clarity and reduces glare in surgical environments. ↩
-
Learn about the hygiene benefits and ease of cleaning that a sealed front surface provides in medical settings. ↩



