A radiologist squints at a CT scan, toggling the window/level settings. The subtle lesion they saw yesterday seems to have vanished, lost in the murky grays of a display that has silently gone out of tune.
*Grayscale curve drift quietly pushes displays off the Digital Imaging and Communications in Medicine (DICOM) Part 14 Grayscale Standard Display Function (GSDF), compressing dark-tone steps and eroding confidence over long sessions; governing targets, stabilization, and routine QA restores predictable perception and fewer rereads while tracking ΔL/JND deviation and recovery time per monitor serial number.**

In radiology, consistent image presentation is not a luxury; it is the foundation of accurate diagnosis. Every diagnostic monitor is calibrated at the factory to the DICOM Part 14 Grayscale Standard Display Function (GSDF), a rule that ensures a uniform relationship between the digital value in an image and the brightness seen on the screen. However, this calibration is not permanent. Over time, every display is subject to "grayscale curve drift1," a slow, subtle degradation that pushes its performance away from this critical standard. This drift is one of the most under-recognized issues in clinical imaging, a silent problem that erodes diagnostic confidence, reduces efficiency, and introduces unnecessary risk. Addressing it requires moving beyond a "set it and forget it" mindset and towards a proactive strategy of governance and technical control; the remedy is auditable GSDF governance with measurable controls.
What “grayscale curve drift” means in clinical reading
A monitor calibrated to the DICOM standard is not a permanent state. Drift is the unseen process that makes that calibration meaningless over time, impacting what a radiologist sees.
*Grayscale curve drift is the deviation of a diagnostic monitor’s luminance response from the DICOM GSDF, collapsing subtle dark-tone steps, compromising diagnostic detail, and forcing fatiguing manual image adjustments; track ΔL/JND deviation and warm-up recovery time (e.g., ≤60 s to target) and log results by monitor serial number.**
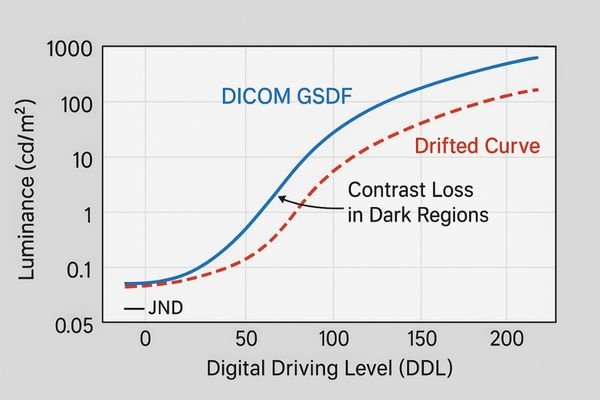
At its core, "grayscale curve drift" is the failure of a diagnostic monitor to maintain its adherence to the DICOM Part 14 Grayscale Standard Display Function (GSDF). The GSDF is a perceptually linearized standard, meaning it is designed so that each step up in a digital grayscale value produces a change in brightness that is equally noticeable to the human eye. This ensures that a subtle finding in a dark area of an image is just as visible as one in a bright area.
The Impact on Just-Noticeable Differences (JNDs)2
When a monitor is new, its luminance output at each grayscale level matches the GSDF curve precisely. As the monitor ages or its temperature fluctuates, this relationship degrades. This is grayscale curve drift. The most common effect is a compression of the dark-end of the curve. Two distinct shades of dark gray that were once clearly different can begin to appear as a single, uniform shade. In effect, the monitor can no longer render all the Just-Noticeable Differences (JNDs) contained in the image data. For a radiologist, this means subtle nodules, faint fractures, or low-contrast lesions may become invisible, forcing them to constantly adjust window and level settings in a frustrating attempt to recover information that the display is no longer capable of showing.
Root causes across devices, rooms, and IT policies
This drift is not caused by a single failure, but by a combination of hardware aging, environmental factors, and a lack of institutional oversight.
Hardware aging, ambient light variations, and inconsistent IT policies without routine QA are the primary causes. Without governance, even identical diagnostic monitors will drift, creating an unreliable imaging environment.
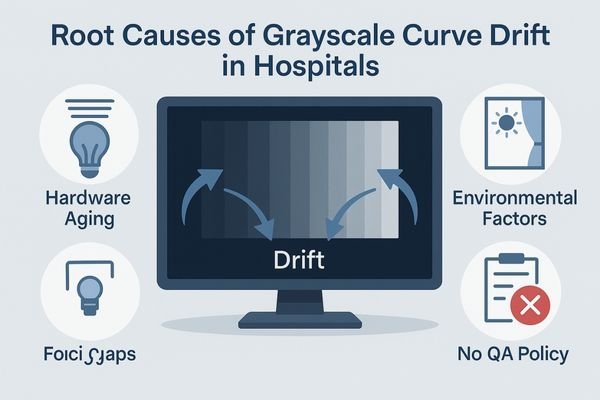
The slow degradation of a monitor’s grayscale performance can be traced to a confluence of factors spanning hardware, the physical environment, and institutional processes; define room-level ambient light limits and calibrated headroom so monitors do not run near maximum luminance for long periods, which accelerates aging.
- Device and Component Aging3: The most fundamental cause is the natural aging of the display’s components. The backlight, whether CCFL or LED, loses brightness over its lifespan. The liquid crystal panel’s transmission properties can change with use and temperature. These physical changes directly alter the monitor’s luminance response, causing it to deviate from its factory-calibrated GSDF curve.
- Environmental Factors: The reading room environment plays a significant role. High or variable ambient light forces radiologists to increase screen brightness to overcome reflections. Running a display at or near its maximum luminance accelerates backlight aging, speeding up drift. Uncontrolled ambient light also changes the viewer’s perceptual adaptation, compounding the effect of any underlying grayscale errors on the display.
- IT and QA Policy Gaps: Perhaps the biggest contributor is the lack of a robust governance policy. Many hospitals operate under the false assumption that DICOM calibration is a one-time event. Without a policy mandating routine, scheduled Quality Assurance (QA) checks, there is no mechanism to detect or correct drift. This policy gap ensures that drift is not only inevitable but also invisible to the organization until it starts causing clinical issues.
Why small grayscale errors create outsized clinical and business risk
A barely perceptible change in grayscale accuracy can have major consequences for patient safety, departmental efficiency, and the hospital’s bottom line.
Small deviations from the GSDF can mask critical, low-contrast findings, leading to missed diagnoses and increased error rates. This drives up reread rates, slows throughput, and erodes clinical confidence; quantify impact via internal service logs and late-shift error statistics in quarterly dashboards.
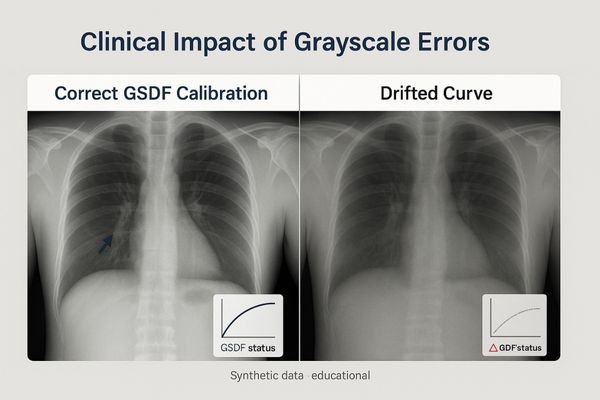
The risks associated with unmanaged grayscale drift are disproportionately large compared to the seemingly small technical error.
Clinical and Quality Risks
The primary risk is to patient safety. A display that can no longer accurately render dark tones may completely obscure low-contrast pathologies. A subtle pneumothorax, a faint fracture line, or the early stages of a soft-tissue tumor can be rendered invisible. This directly increases the risk of a missed or delayed diagnosis. As radiologists unconsciously lose confidence in what their screens are showing them, they begin to compensate by spending more time on each study, performing more rereads, and adjusting window/level settings more frequently. This not only causes fatigue but also directly harms departmental productivity.
Business and Operational Risks
From a business perspective, drift introduces unpredictability. If the quality of image perception changes from one workstation to another, or even on the same workstation from morning to afternoon, it becomes impossible to manage quality or throughput effectively. This unpredictability leads to an increase in IT support tickets as frustrated clinicians report "image quality issues4" without a clear cause. It creates a "no-fault" failure mode that burns valuable time from both clinical and technical staff, driving up operational costs. Define a service-level agreement for GSDF governance—ticket resolution time limits, quarterly GSDF pass-rate targets, and cross-room perception consistency—to restore predictability.
A pragmatic GSDF governance strategy you can audit
The solution is to replace assumptions with a disciplined, auditable strategy that actively manages grayscale performance from procurement to disposal.
*Define a GSDF compliance target, use diagnostic monitors with built-in stabilization, perform routine automated QA with logging, and establish a clear protocol for correcting any detected deviations; specify JND/ΔL thresholds and maximum warm-up recovery time, and maintain a shared audit log.**

An effective GSDF governance strategy5 is built on a simple principle: "trust, but verify." It involves establishing clear standards and then using technology and process to ensure they are consistently met.
- Define a Target and Policy: Set GSDF conformance as the standard for all diagnostic monitors and define pass/fail in JND/ΔL* terms, including an allowed post–warm-up recovery time threshold.
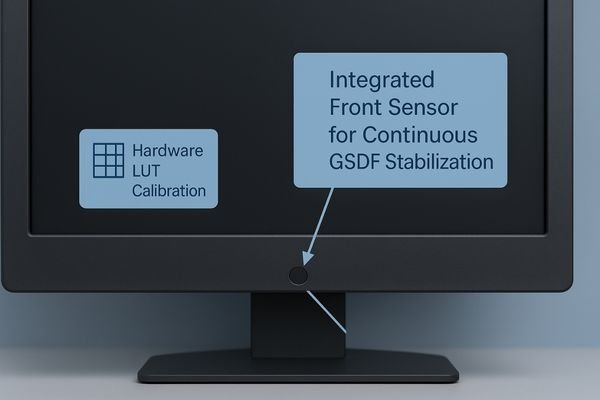
- Automate Stabilization: Mandate diagnostic monitors with integrated front sensors and automatic luminance stabilization to counter warm-up and short-term fluctuations; control GPU LUTs and EDID so OS/apps cannot silently alter the grayscale response.
- Implement Auditable QA: Use network-based software to run regular GSDF tests, log results centrally by serial number (ΔL*/JND curve + timestamp), and flag out-of-tolerance devices; adopt TG18/SMPTE test charts for cross-site acceptance and record pass/fail to a shared log.
- Establish a Correction Protocol: Apply a unified cadence—baseline at install; monthly automated conformance checks; quarterly manual verification with test patterns; immediate recheck after panel/firmware changes or alarms; annual full calibration—and define steps for remote recalibration or replacement when flagged.
Selection principles for drift-resistant diagnostic monitors
Choosing the right hardware is the foundation of a successful governance strategy. A display’s design determines whether stable performance is achievable.
Prioritize diagnostic monitors with integrated front sensors for auto-stabilization, hardware LUT calibration, detailed factory conformance reports, and sufficient brightness headroom; require predictable EDID behavior, dual-input comparison modes, and acceptance records for source-to-monitor matching.
When procuring new diagnostic monitors, the selection criteria must go beyond just resolution and size. To build a drift-resistant fleet, focus on the features that enable long-term grayscale stability.
Key Selection Criteria
The most critical feature is an integrated stabilization system, typically a front sensor paired with a backlight sensor, that provides continuous, real-time correction to maintain both brightness and GSDF conformance. The monitor must also support hardware-level Look-Up Table (LUT) calibration6, which allows for corrections to be written directly to the display’s hardware, ensuring accuracy that is independent of the host PC. Insist on receiving a detailed factory calibration and conformance report with each monitor, documenting its adherence to DICOM GSDF at the time of manufacture; the report should include target luminance, GSDF curve, a uniformity map, measurement date, and instrument details. Finally, select monitors with significant luminance headroom—a maximum brightness well above the intended calibrated brightness. This headroom allows the stabilization system to compensate for natural backlight aging over many years, dramatically extending the display’s usable life at its target performance level.
Recommended Drift-Resistant Diagnostic Monitors
| Model | Score | Suitability for GSDF Governance |
|---|---|---|
| MD33G | 87/100 | General PACS rooms; GSDF-capable hardware calibration and luminance stabilization. |
| MD52G | 90/100 | High-precision grayscale tasks; ample headroom and documented uniformity. |
| MD120C | 88/100 | Unified 12MP canvas; stable luminance and acceptance logs simplify governance. |
Business value: stabilized perception, fewer tickets, longer life
A strong GSDF governance strategy pays for itself through increased efficiency, lower operational costs, and smarter capital asset management.
Stabilized perception improves throughput and reduces rereads; proactive QA cuts IT tickets and troubleshooting costs, while brightness headroom extends usable life—track reread rate, average report turnaround, color/gray-related ticket counts, and average closure time before/after deployment to quantify ROI.
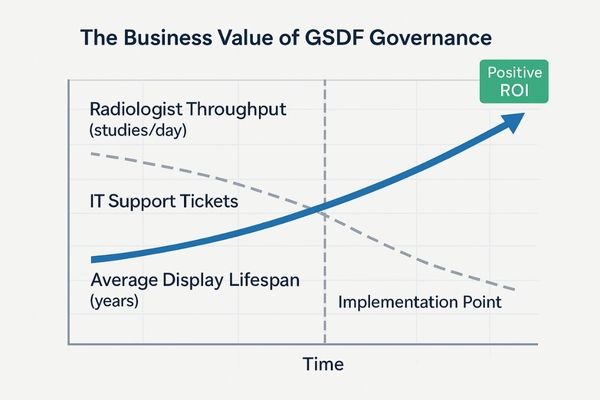
The business case for implementing and enforcing a GSDF governance strategy is robust. The investment in appropriate technology and process delivers returns across multiple areas of the organization. Firstly, it enhances clinical productivity. When radiologists can trust that every diagnostic monitor is perceptually identical, they read with greater confidence and speed, improving departmental throughput. Secondly, it drastically reduces operational costs. Proactive, automated QA all but eliminates the frustrating and time-consuming "image quality" support tickets that drain resources from both the radiology and IT departments. Finally, it optimizes capital expenditure. By selecting monitors with the technical ability to maintain their performance over a long period, the hospital can extend its replacement cycle. This avoids premature, "complaint-driven" upgrades and lowers the total cost of ownership for the entire display fleet, allowing for more strategic and predictable asset management.
FAQ: thresholds, cadence, and multi-monitor matching
What is an acceptable threshold for GSDF drift?
While guidance such as the American Association of Physicists in Medicine (AAPM) Task Group 18 (TG-18) is often referenced, define pass/fail primarily in **JND/ΔL*** terms (record percent luminance deviation only as a reference) and link thresholds to room ambient light and warm-up recovery time.
How often should we run QA tests?
Adopt a unified cadence: baseline at installation; monthly automated conformance checks; quarterly manual verification with test patterns; immediate recheck after panel or firmware changes or alarms; and annual full calibration.
How do we ensure multi-monitor workstations are matched?
Start with identical diagnostic monitors. Use QA software to calibrate all displays on a workstation to the same target luminance and GSDF curve simultaneously; built-in stabilization then maintains the match between scheduled QA checks.
Conclusion
By governing GSDF targets with stabilized diagnostic monitors and routine QA, hospitals can eliminate grayscale drift, restore predictable perception, and ensure long-term diagnostic confidence and efficiency. To request a GSDF governance checklist and acceptance templates, contact info@reshinmonitors.com. This article covers display/QA governance and does not constitute medical advice.
-
Exploring the causes of grayscale curve drift can help improve monitor calibration and maintain diagnostic accuracy. ↩
-
Exploring JNDs can enhance your knowledge of image perception and its impact on radiology. ↩
-
Understanding this concept is crucial for maintaining optimal monitor performance and longevity. ↩
-
This link will help you understand strategies to tackle image quality issues, improving diagnostic accuracy and operational efficiency. ↩
-
Explore this link to understand the principles and practices that ensure effective GSDF governance. ↩
-
Exploring this topic will help you grasp how calibration enhances display accuracy and reliability. ↩



