A surgeon glances between an endoscopic view and a radiological scan on adjacent monitors, but the anatomy looks different. This forces a moment of hesitation—a moment where clinical confidence is lost.
Multi-monitor comparisons often expose subtle mismatches that snowball into clinical risk. Standardize GSDF and luminance stability, lock signal paths and EDID, use fixed multiview layouts, and control ambient light with auditable QA to make decisions faster and safer.

In modern ORs and reading rooms, multi-monitor views1 are essential for correlating modalities and timelines. Yet unless displays are synchronized, this “bigger picture” becomes a fractured one. This article defines what counts as inconsistency, quantifies its clinical risks2, and provides a deterministic, auditable path to fix it.
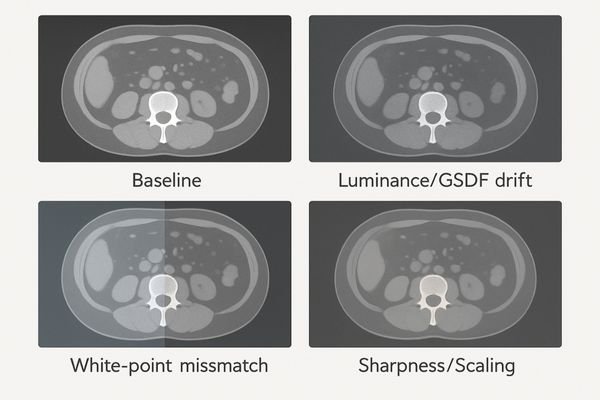
What counts as multi-monitor inconsistency
Inconsistency is not just about one screen being brighter than another—it’s a set of deviations that make the same case look different across displays. Common offenders include:
- Luminance and GSDF: target GSDF error within ±5%.
- Color/white-point: differences that shift tissue appearance.
- Spatial issues: non-uniformity ≤15%, scaling artifacts, incorrect pixel mapping.
- Temporal issues: processing latency differences that desynchronize views.
- Signal path: bit-depth/chroma/EDID not matched across outputs.
Clinical risks and workflow impact
When displays diverge, clinicians must compensate mentally for technical flaws instead of focusing on the patient. Risks include:
- Hidden findings/misreads3: low-contrast lesions may vanish on one display.
- Hand–eye disruption4: latency or color differences in surgery degrade coordination.
- Divergent reports: teams “see” different things and debate grows.
- Rework and delays: lower throughput and eroded confidence in equipment.

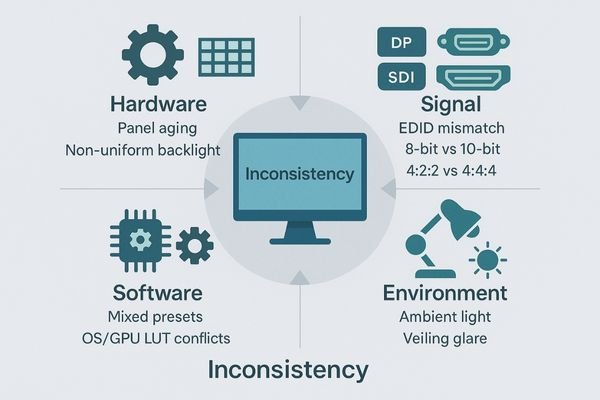
Main causes across hardware/software/environment
Inconsistency is systemic—rarely a single bad monitor:
- Hardware: panel aging without luminance stabilization5, uneven backlight, poor uniformity.
- Signal: wrong bit-depth/chroma, unstable or mismatched EDID, converters/cables that cap bandwidth.
- Software: mixed viewer presets, OS/GPU LUT conflicts, unmanaged color pipelines6.
- Environment: uncontrolled ambient light, veiling glare, non-standardized presets between users.
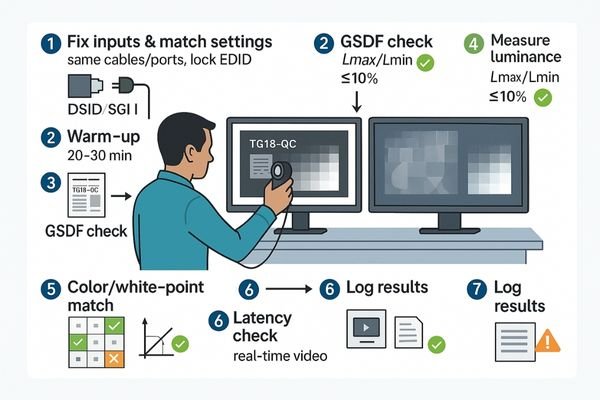
Side-by-side verification steps
Verifying consistency is objective—not an eyeball test. Use standardized patterns and instruments:
- Fix inputs & match settings: identical cables/ports; same resolution, refresh, bit-depth and chroma for both outputs; lock EDID.
- Warm-up: both displays typically 20–30 min to reach thermal/luminance stability.
- GSDF check7: with TG18-QC (or equivalent). Target GSDF error ≤ ±5% across the curve.
- Measure luminance: Lmax/Lmin and stability (ΔL/L ≤ 10%); record results.
- Uniformity: multi-point test with ≤15% max deviation across the panel.
- Color/white-point: match coordinates for color-critical use; document results.
- Latency check8: for real-time video (endoscopy/OR), confirm no perceptible lag.
- Log everything: store measurements and dates to build an auditable QA history.
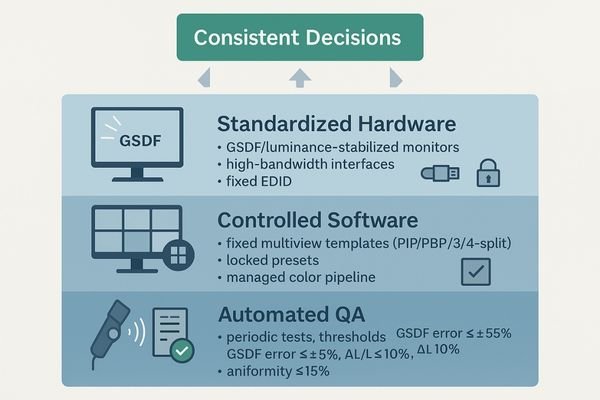
Solution: build a deterministic, auditable display pipeline
A durable fix comes from system design, not one-off tweaks:
- Standardize GSDF + luminance stabilization9: continuously counter panel aging.
- Lock signal paths: use high-bandwidth interfaces (12G-SDI / DisplayPort), fixed EDID, and controlled bit-depth.
- Use fixed multiview templates: PIP/PBP/3-split/4-split. On a 4K screen, a 4-way quad yields roughly 4×1080p panes.
- Control ambient light: target 20–40 lux in reading rooms/ORs; minimize veiling glare.
- QA automation10: periodic tests, threshold alerts, and signed logs for medico-legal defensibility.
Recommended models aligned to this workflow:
| Model | Primary Scenario | Multi-view / QA Relevance |
|---|---|---|
| MS321PB | Endoscopy / OR cart | PIP/PBP/3-split/4-split; AR-bonded glass; stable 4K consistency |
| MS322PB | 32″ 4K surgical monitor | PIP/PBP/3-split/4-split; BT.2020; optical bonding; easy sanitizing |
| MS550P | 55″ wall display / hybrid OR | Large-screen quad view; PIP/PBP/3-split/4-split; BT.2020 |
| MD52G | 5MP diagnostic (CT/MR/DR) | DICOM Part 14, automated stabilization, ΔL/L governance |
| MD85CA | 8MP multimodality / tumor board | Up to 8-window multi-source, DICOM QA, ambient compensation |
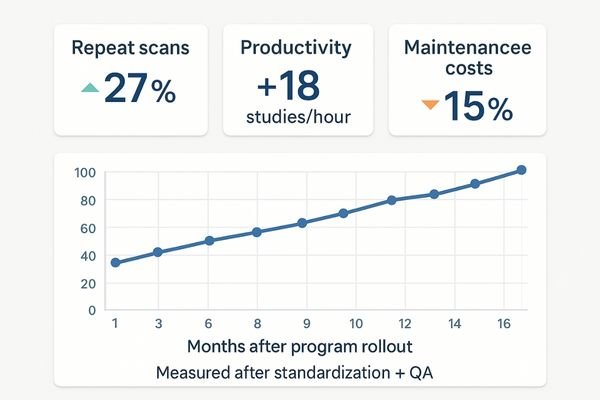
Business value and measurable ROI
A consistent pipeline delivers measurable returns:
- Fewer misreads & repeats11: less radiation exposure and lower imaging costs.
- Faster consensus: higher reading room throughput; shorter procedures in ORs.
- Lower TCO12: extended panel life, proactive maintenance, fewer on-site calls.
- Onboarding & cross-team clarity: fixed templates and shared visual baselines.
FAQ: practical implementation answers
-
Is a one-time calibration enough?
No. Displays drift with aging and environment. Combine initial calibration with continuous luminance stabilization and scheduled QA logging. -
Can we mix brands and still keep consistency?
Yes—if you enforce one baseline (GSDF/white point/gamma), lock EDID/bit-depth, and audit with the same thresholds for every unit. -
How much detail remains in a 4K quad-view?
Roughly four 1080p panes. Ensure each source is ≥1080p and that the multiview scaler preserves detail. -
What uniformity and stability numbers should we target?
Uniformity ≤15%, ΔL/L ≤10%, and GSDF error ≤ ±5%, with ambient 20–40 lux. -
Which interfaces reduce surprises in the OR?
Prefer 12G-SDI for long, deterministic runs and DisplayPort for near-field low latency; keep paths short and audited. -
How do we prevent settings drift by different users?
Lock read-only presets, restrict local OSD changes, and use centralized QA software to push/verify configurations.
Conclusion
Consistency isn’t a feature—it’s a system. By standardizing GSDF and luminance stability, locking signal paths and EDID, enforcing fixed multiview templates, and controlling ambient light with auditable QA, you turn perception into data and de-risk clinical decisions.
Need a reproducible multiview baseline in your OR or reading room? Email info@reshinmonitors.com for a quick audit checklist.
-
Explore how multi-monitor views enhance efficiency and accuracy in modern operating rooms. ↩
-
Understanding clinical risks can help improve patient safety and outcomes in healthcare environments. ↩
-
Understanding hidden findings can enhance diagnostic accuracy and improve patient outcomes. ↩
-
Exploring hand-eye disruption can help improve surgical techniques and coordination. ↩
-
Understanding panel aging can help you maintain monitor quality and improve visual consistency. ↩
-
Exploring unmanaged color pipelines can enhance your knowledge of color accuracy and improve your workflow. ↩
-
Understanding GSDF checks is crucial for ensuring display accuracy and quality in critical applications. ↩
-
A latency check is essential for real-time applications; exploring this will enhance your understanding of display performance. ↩
-
Understanding GSDF and luminance stabilization can enhance your knowledge of display technology and improve system design. ↩
-
Exploring QA automation can provide insights into effective quality control practices and enhance your project’s reliability. ↩
-
Explore how minimizing misreads can enhance patient safety and reduce costs in healthcare. ↩
-
Learn about strategies to reduce TCO and improve financial efficiency in medical equipment management. ↩



