High-touch surfaces in medical settings are breeding grounds for bacteria, posing a constant risk of healthcare-associated infections. Choosing the right protective technology is critical for patient and staff safety.
In the field of medical-grade displays, antibacterial protection is increasingly achieved through two leading technologies: silver ion antibacterial coating and photocatalytic antibacterial coating. Silver ion coatings provide continuous and stable defense through ion-based sterilization, while photocatalytic coatings utilize light activation to deliver highly effective antibacterial performance. Each offers distinct advantages in durability, adaptability, and maintenance. As global healthcare systems place greater emphasis on infection control and device safety, these coatings are becoming essential innovations driving the reliability and performance of medical-grade displays.
The push for enhanced infection control in clinical environments has brought surface technology to the forefront. Medical displays, which are frequently touched by multiple users throughout the day, require robust protection against microbial contamination. Two leading solutions have emerged to meet this challenge: silver ion (Ag⁺) coatings1 and photocatalytic coatings2. While both aim to create a self-disinfecting surface, their underlying technical mechanisms and performance characteristics differ significantly. Understanding these distinctions is crucial for selecting equipment that provides reliable protection in its intended clinical setting. This article provides a comparative analysis of these two technologies, exploring their antibacterial mechanisms, durability, safety, and suitability for various medical environments.
Antibacterial Mechanism Differences
Not all antibacterial coatings are created equal. Choosing a technology without understanding its mechanism can lead to ineffective protection in certain environments, undermining infection control efforts.
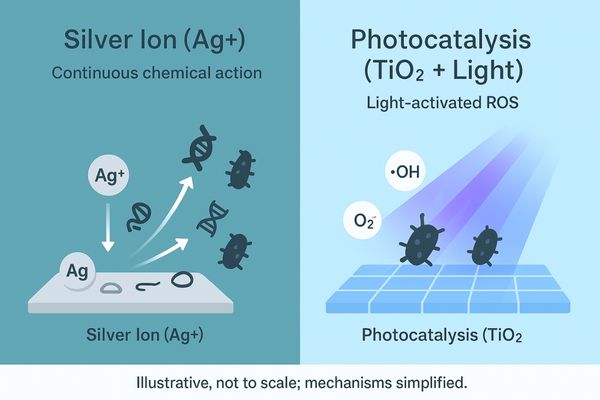
Silver ion coatings work by releasing ions that disrupt multiple bacterial cell functions for continuous sterilization. Photocatalytic coatings use light to generate highly reactive oxygen species that destroy pathogens on contact.
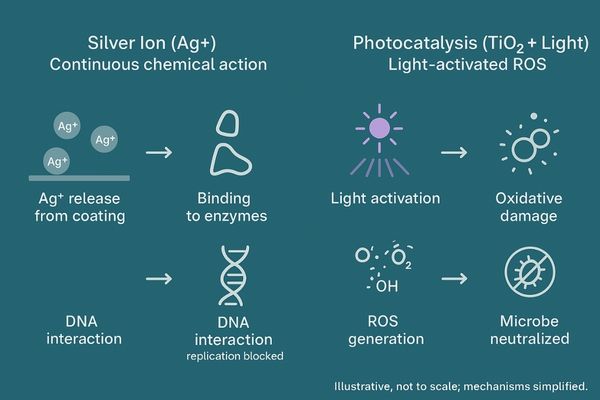
The core distinction between these technologies lies in how they neutralize pathogens. Silver ion coatings employ a multi-modal chemical attack. The coating continuously releases silver ions (Ag⁺), which bind to thiol groups in the enzymes of a microbe, disrupting its metabolism and respiratory functions. The ions also penetrate the cell wall to interact with DNA, blocking replication and protein synthesis, which ultimately leads to cell death. This multi-target mechanism is effective against a broad spectrum of microbes, including Gram-positive and Gram-negative bacteria, and makes it difficult for them to develop resistance. In contrast, photocatalytic coatings3, typically using titanium dioxide (TiO₂), are driven by photochemical reactions. When illuminated by UV or high-energy visible light, the coating generates powerful reactive oxygen species (ROS) like hydroxyl radicals (•OH) and superoxide anions (O₂⁻). These ROS aggressively oxidize the organic components of microbes, destroying their cell membranes and vital internal structures.
Durability and Cleaning Resistance
Medical equipment undergoes rigorous and frequent cleaning. A coating that degrades or wears off fails to provide the long-term protection required in a clinical setting.
Silver ion coatings can be highly durable, but their active agent may deplete over time. Photocatalytic coatings are theoretically permanent but can be rendered ineffective if the surface is damaged or fouled.

The longevity of these coatings presents a key trade-off. For silver ion coatings4, effectiveness depends on the sustained release of Ag⁺. While advanced formulations embed silver robustly to withstand thousands of cleaning cycles, the reserve of silver is finite. Real-world studies, such as those on high-touch smartphone screens, have shown that antimicrobial efficacy can diminish over a month as the surface ions are depleted. This means that after prolonged, intensive use, the coating’s performance may eventually decline. On the other hand, the photocatalyst in a TiO₂ coating5 is not consumed in the reaction, giving it a theoretically indefinite lifespan. As long as the surface remains intact and exposed to light, it can continuously generate ROS. The primary risk is not depletion but degradation. Harsh physical abrasion can damage the coating, and certain cleaning agents containing siloxanes can leave an invisible film that blocks light, temporarily deactivating the surface until it is thoroughly cleaned again.
Safety and Biocompatibility
Introducing any new material into a clinical setting demands absolute certainty about its safety. An antibacterial solution cannot be effective if it poses any risk to patients or staff.
Both silver ion and photocatalytic coatings are proven to be safe and biocompatible for medical use. Silver ion release is controlled to remain far below toxicity levels, and both materials meet stringent safety standards.
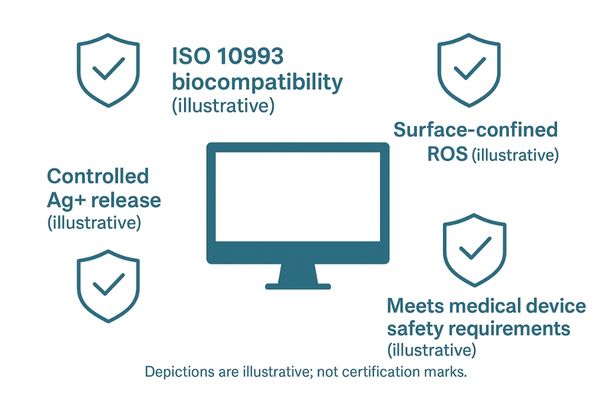
Both technologies have an excellent safety profile, validated by extensive use and regulatory oversight. Silver has a long history in medical applications6 like wound dressings. In a display coating, the Ag⁺ ion release rate is carefully engineered to be lethal to microbes while remaining well within safe limits for human contact. At these low concentrations, the risk of cytotoxicity is negligible. Titanium dioxide, the basis for most photocatalytic coatings7, is a chemically inert mineral designated as Generally Recognized As Safe (GRAS) by the FDA. The ROS it generates are confined to the immediate surface of the coating and have an extremely short lifespan, posing no threat to human tissue upon incidental contact. The primary safety consideration during manufacturing is managing loose nanoparticles, but once cured into a solid film, the particles are fixed and stable. Both technologies comply with medical device regulations like ISO 10993, ensuring they are biocompatible and safe for clinical environments.
Adaptability in Different Medical Environments
A hospital contains diverse environments, from brightly lit wards to dark operating theaters. A one-size-fits-all approach to antibacterial protection may not be effective across all these settings.
Silver ion coatings offer consistent, light-independent protection ideal for high-risk areas like ICUs and ORs. Photocatalytic coatings are highly effective in well-lit spaces like consultation rooms and nurses’ stations.

The optimal choice of coating depends entirely on the specific clinical environment. I see three primary scenarios where the technical differences become critical:
Intensive Care Unit (ICU)
In the ICU, continuous microbial control is paramount. Lights are often dimmed for patient rest, creating conditions where a photocatalytic coating8 would be inactive. Silver ion coatings are far better suited here, as they provide around-the-clock passive protection regardless of lighting. This ensures constant, reliable defense at the bedside.
Operating Room (OR)
The OR is typically intensely lit, which can supercharge a photocatalytic coating, allowing it to actively neutralize microbes in real-time during a procedure. However, for this to work, the coating must be a newer formulation responsive to visible light, as standard TiO₂ requires UV. A silver ion coating also performs well, offering immediate action against any contaminants.
Radiology Reading Room
These rooms are kept dark to optimize image viewing, rendering photocatalytic coatings almost entirely useless. A silver ion coating is the clear choice, as it functions perfectly in the dark to suppress bacteria on frequently touched screens.
Dependence on Light and Environmental Conditions
An ideal solution should perform reliably under the real-world conditions of a busy hospital. An agent’s effectiveness should not be compromised by its immediate environment.
Silver ion coatings are not dependent on light, ensuring reliable and continuous antibacterial performance. Photocatalytic coatings depend on both light spectrum and intensity, making their performance highly variable by location.
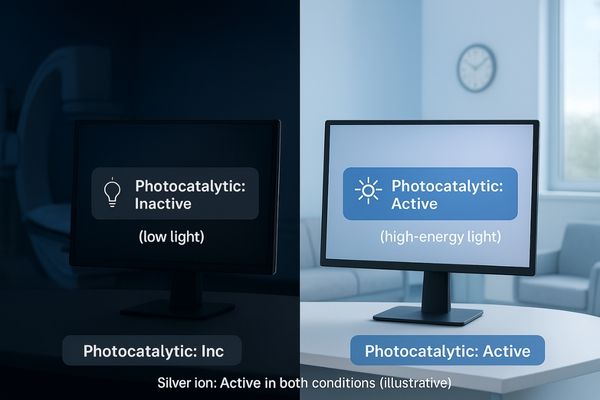
The most significant operational difference is environmental dependence. Silver ion technology9 is environment-agnostic. Its bactericidal action is an inherent chemical property that functions consistently in light or darkness, at any normal room temperature or humidity. This makes it a robust and predictable solution for any department. In contrast, photocatalytic coatings10 are highly dependent on light. Their performance is dictated by two factors: spectrum and intensity. Conventional TiO₂ requires UV light, which is absent in most indoor lighting. Newer, doped photocatalysts can be activated by high-energy visible light (like 405 nm violet-blue light), but performance still scales with intensity. Under bright surgical lamps, the effect is powerful; in a dimly lit corner of a ward, it may be negligible. This "active when lit, dormant when dark" nature means its application must be carefully matched with the ambient lighting conditions of its intended location.
Ease of Cleaning and Maintenance
Hospital cleaning protocols are stringent and non-negotiable. Any surface coating must be compatible with standard procedures without requiring special treatment that could disrupt workflows.
Silver ion coatings are highly resistant to common hospital disinfectants. Photocatalytic coatings require more care, as some cleaners leave residues that can deactivate the surface by blocking light.

From a maintenance perspective, silver ion coatings11 offer greater simplicity. They are compatible with standard hospital disinfectants, including alcohol and bleach-based solutions. Staff can follow existing protocols without fear of damaging the coating or its efficacy, making it easy to integrate into existing workflows. The primary advice is to use non-abrasive cloths to prevent scratching. Photocatalytic coatings require more careful consideration. While the TiO₂ material itself is chemically inert, its function can be impeded. Cleaners containing waxes or silicones can leave behind a microscopic film that blocks light from reaching the catalyst, effectively turning it off. This film must be removed with a solvent like alcohol to restore function. On the plus side, photocatalytic surfaces are often hydrophilic and can exhibit a "self-cleaning" property, breaking down organic grime like fingerprints under illumination, which can make them easier to wipe clean. However, the need to avoid certain common cleaning agents adds a layer of complexity to maintenance routines.
Real-World Applications and Case Studies
Theoretical benefits must be backed by real-world evidence. Clinical evaluations demonstrate the practical impact of these technologies on infection control and hospital safety.
Case studies confirm the efficacy of both technologies in their ideal settings, but also highlight the potential for silver ion depletion and the critical need for proper lighting to activate photocatalytic surfaces.
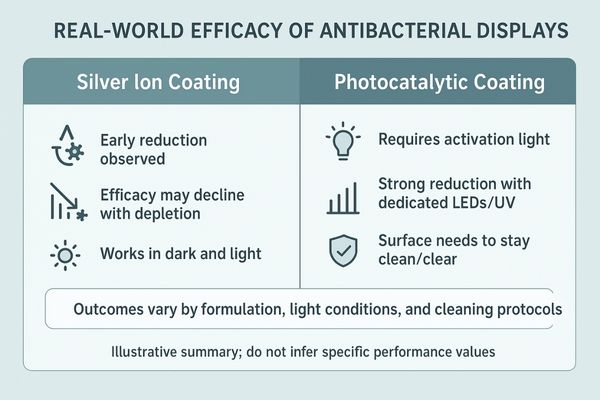
Clinical studies provide valuable context. For silver ion coatings12, one real-world evaluation on physicians’ smartphones found that an antimicrobial glass cover reduced bacterial diversity in the first week, but its effect diminished by day 30, suggesting potential ion depletion on high-contact surfaces. This highlights the importance of robust formulations for long-term efficacy. For photocatalytic technology13, a study in a hematology ward using a TiO₂-based air and surface sanitizer activated by LEDs showed striking results. It not only reduced the environmental microbial load but also led to a statistically significant decrease in patient infections. This confirms the powerful potential of photocatalysis when implemented with a dedicated light source. These studies validate the core strengths of each technology but also underscore their limitations.
Conclusion
Both silver ion and photocatalytic coatings offer powerful tools for infection control, but their distinct mechanisms and operational requirements demand careful consideration for each clinical application.
📧 Want guidance on selecting the right antimicrobial coating for your medical displays? Contact Martin at martin@reshinmonitors.com to explore Reshin’s tailored solutions.
-
Explore how silver ion coatings can enhance infection control in clinical settings, ensuring safer environments for patients and staff. ↩
-
Learn about the innovative photocatalytic coatings that provide self-disinfecting surfaces, improving hygiene in medical facilities. ↩
-
Learn about the innovative mechanisms of photocatalytic coatings and their effectiveness in destroying microbes. ↩
-
Explore this link to understand the effectiveness and limitations of silver ion coatings in various applications. ↩
-
Discover the unique properties of TiO₂ coatings and their long-lasting benefits for antimicrobial surfaces. ↩
-
Explore this link to understand how silver is utilized in medical applications, enhancing safety and efficacy in treatments. ↩
-
Discover the science behind photocatalytic coatings and their role in improving medical device safety and performance. ↩
-
Learn about the effectiveness of photocatalytic coatings in high-light environments and their role in real-time microbial neutralization. ↩
-
Explore this link to understand the unique benefits of Silver ion technology in various applications. ↩
-
Discover the potential and limitations of photocatalytic coatings in different lighting conditions. ↩
-
Explore the advantages of silver ion coatings for healthcare settings, including their compatibility with disinfectants and ease of maintenance. ↩
-
Explore this link to understand how silver ion coatings enhance antimicrobial protection in healthcare environments. ↩
-
Discover the impact of photocatalytic technology on infection control and patient safety in clinical settings. ↩



