The pandemic pushed many fields online. Is breast radiology one of them? Can crucial diagnoses happen remotely without compromising care? Let’s explore.
Telework in breast radiology means radiologists interpret mammograms and other breast studies remotely. This requires specialized high-resolution displays, secure connections, and strict protocols. It ensures diagnostic accuracy even outside the hospital.

The COVID-19 pandemic certainly accelerated changes in how medical professionals work. Teleradiology, which is reading medical images remotely, saw a huge surge. It allowed many diagnostic services to continue when physical presence was difficult.
However, not all areas of radiology are equally suited to remote work without careful consideration. Breast imaging, for instance, has incredibly high demands for image quality. Many people ask me, "Can a radiologist truly read a mammogram1 accurately from their home office?" It’s a valid question. The answer involves a deep dive into technology, workflow, and unwavering commitment to quality. Let’s look at the specific aspects of telework in breast radiology.
Introduction – The rise of telework in radiology after COVID-19
Work changed suddenly for many. Radiology faced new pressures. How did remote work become so common in this field?
COVID-19 forced radiology departments to adopt telework rapidly. This maintained essential diagnostic services during global disruptions. It showed remote reading was possible, but also highlighted its specific needs.
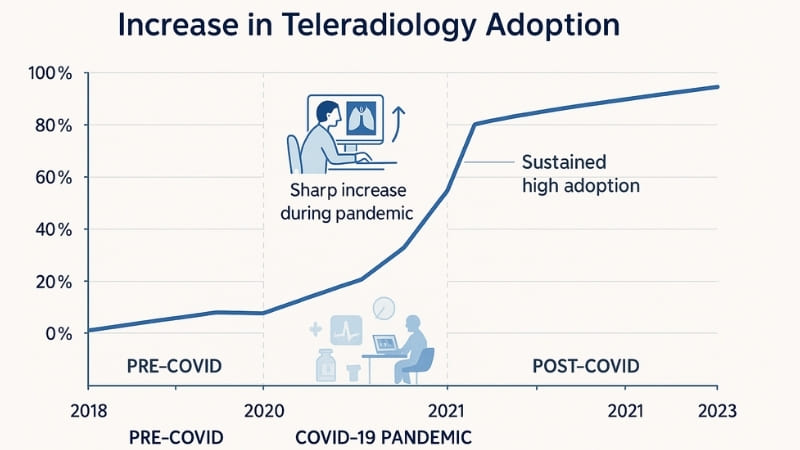
Before the pandemic, teleradiology2 was already established in some areas. It helped provide coverage for smaller hospitals or after-hours services. However, for many larger institutions and specialized fields, it was not the primary mode of operation. COVID-19 changed that almost overnight. Social distancing and lockdown measures meant we needed new ways to keep healthcare running. Radiology departments had to quickly figure out how their teams could work remotely. This rapid shift was a major undertaking. It involved setting up secure connections, deploying appropriate hardware to radiologists’ homes, and adapting workflows. We saw firsthand at Reshin how demand for medical-grade displays3 suitable for remote diagnosis4 surged. This period truly tested the capabilities of teleradiology. It also forced a broader acceptance and understanding of its potential to ensure continuity of care and provide flexibility for medical staff. The experience gained has shaped how we view remote diagnostics today.
Why breast imaging presents unique challenges for remote interpretation
Reading breast images remotely sounds simple. But tiny details matter greatly. What makes breast imaging so tough for telework?
Breast imaging demands detection of minute details like microcalcifications. Mammograms are complex. They need ultra-high-resolution, specially calibrated monitors. Replicating ideal hospital viewing conditions at home is a significant challenge.
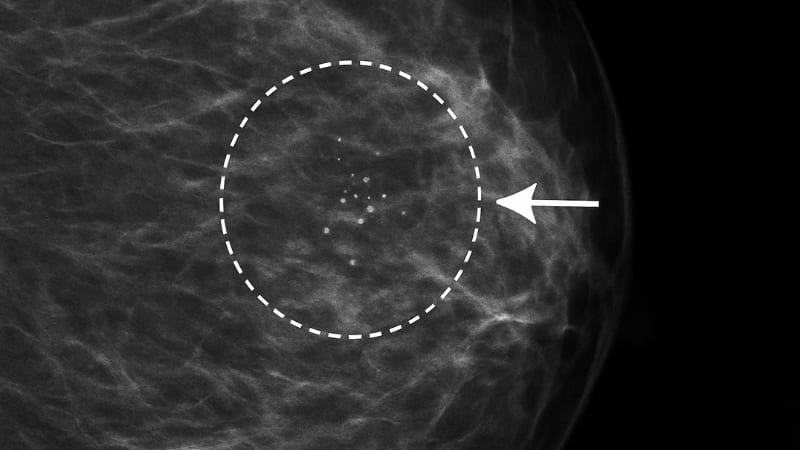
Breast imaging is one of the most demanding areas in radiology. Radiologists are looking for incredibly subtle signs of cancer. These can include tiny specks called microcalcifications, which can be smaller than a grain of salt. They also look for faint distortions in breast tissue or slight differences in density. My first personal insight is crucial here: Breast radiology demands extremely high image fidelity5 — telework setups must never compromise on display quality. I always emphasize 5MP or higher, DICOM-calibrated monitors for remote reads6. Mammography images, especially digital breast tomosynthesis (DBT or 3D mammography)7, are very large files with a huge amount of data. DBT involves multiple image slices, requiring the radiologist to scroll through them. This demands not only a high-resolution display but also a powerful workstation. Furthermore, comparing current images to prior studies is essential in breast imaging. This means the remote setup must seamlessly integrate with the hospital’s Picture Archiving and Communication System (PACS). The challenge is to ensure that these critical details are just as visible on a remote workstation as they would be on a dedicated review station in the hospital.
Unique Demands of Breast Imaging
| Challenge Area | Specific Issue | Implication for Remote Reading |
|---|---|---|
| Image Detail | Detection of tiny microcalcifications, subtle masses. | Requires very high-resolution medical displays. |
| Image Type | Dense breast tissue, large DBT file sizes. | Needs powerful workstations, high bandwidth. |
| Comparison | Essential to compare with multiple prior studies. | Requires fast, reliable PACS access. |
| Viewing Conditions | Standardized low ambient light in hospital reading rooms. | Difficult to consistently replicate at home. |
| Diagnostic Confidence | High stakes – early cancer detection. | No compromise on image quality or setup is acceptable. |
These factors make remote breast imaging a specialized task, not suited for standard computer equipment.
The technical requirements for effective remote breast image reading
Want to read mammograms at home? A regular computer screen won’t do. What specific technology is essential for accuracy?
Effective remote breast reading needs medical-grade displays of at least 5 Megapixels. These must be DICOM calibrated for accurate grayscales. Secure, fast network access and controlled ambient lighting are also vital.

To ensure that remote breast image interpretation is safe and effective, the technical setup must be impeccable. It’s not just about having a screen; it’s about having the right screen and the right environment. First, the display itself is paramount. As I mentioned, we recommend a minimum of 5 Megapixel (5MP) resolution8 for mammography. For tomosynthesis, even higher resolutions or dual 5MP setups are common. These monitors must be medical-grade, specifically designed for diagnostic imaging. My second personal insight here is stark: Consumer-grade displays are not an option. Even if remote work is flexible, diagnostic accuracy isn’t — subtle microcalcifications can’t be missed. These medical displays offer higher brightness, better contrast, and are calibrated to the DICOM GSDF (Grayscale Standard Display Function) standard. This ensures that images are displayed consistently and accurately, just as they would be in the hospital.
Then there’s the environment. My third insight is equally critical: Lighting control9 is as important at home as in the hospital. Ambient light ruins grayscale perception. A proper reading room setup is non-negotiable. This means minimizing glare and reflections on the screen. Secure, high-speed internet is also non-negotiable. My fourth insight points to this: Bandwidth and image delivery systems must support lossless transmission. Breast images often have large file sizes — any compression risks losing clinical detail. The workstation needs to be powerful enough to handle large image datasets smoothly.
Essential Tech for Remote Breast Reading
| Component | Minimum Specification / Requirement | Why It’s Critical |
|---|---|---|
| Display Monitor | Medical-grade, 5MP+ resolution, DICOM Part 14 calibrated | Ensures visibility of fine details, accurate grayscales. |
| Workstation CPU/GPU | High-performance, sufficient RAM | Smooth handling of large image files (especially DBT). |
| Network Connection | High-speed, stable, secure (VPN, encryption) | Fast image loading, protection of patient data (HIPAA/GDPR). |
| Reading Environment | Low ambient light (typically <50 lux), ergonomic setup | Optimizes image perception, reduces eye strain. |
| Software | Calibrated viewing software, PACS integration | Correct image presentation, access to priors. |
These are not just recommendations; they are foundational requirements. Someone like Dr. Amy Chen, who focuses on surgical visualization and equipment integration, would appreciate this level of technical rigor, as similar principles of image integrity apply across medical specialties.
Benefits and limitations of telework in breast radiology?
Is remote breast imaging a perfect solution? It offers new freedoms. But what are the potential drawbacks to consider carefully?
Benefits of telework in breast radiology include radiologist flexibility and wider access to subspecialists. Limitations involve maintaining quality control, IT support challenges, and potential for reduced team collaboration.
Telework in breast radiology, when implemented correctly, offers several compelling advantages. One of the most significant is flexibility for radiologists. This can improve work-life balance and potentially reduce burnout. It can also expand access to subspecialist breast imagers. A clinic in a remote area could have its studies read by an expert hundreds of miles away. This can lead to improved diagnostic accuracy and better patient outcomes in underserved regions. Teleradiology can also facilitate load balancing between different sites and potentially increase productivity by minimizing interruptions common in a busy hospital department.
However, there are also limitations and challenges that must be managed. Maintaining consistent image quality and adherence to strict viewing protocols across multiple remote locations is a primary concern. Providing robust IT support for home workstations can be complex and costly. Data security and patient privacy (ensuring HIPAA or GDPR compliance) are paramount and require careful attention. Another consideration is the potential for reduced interaction among colleagues. Those spontaneous case discussions or second opinions that happen organically in a shared reading room can be lost. This requires proactive measures to facilitate collaboration, such as regular virtual meetings or easy-to-use image sharing tools for consultation.
Weighing Pros and Cons
| Aspect | Benefit | Limitation / Challenge |
|---|---|---|
| Workforce | Increased radiologist flexibility, job satisfaction. | Potential for isolation, reduced team interaction. |
| Access to Care | Extends subspecialist expertise to remote areas. | Relies on robust internet infrastructure everywhere. |
| Quality Control | If well-managed, can maintain standards. | Harder to monitor remote environments, ensure compliance. |
| Cost | Potential travel savings for radiologists. | High cost of equipping home stations to medical standards. |
| Efficiency | Fewer interruptions can boost productivity. | Time lost to technical issues if IT support is slow. |
A successful tele-breast-radiology program carefully addresses these limitations.
Personal Thoughts – What matters most when choosing displays for remote breast reading
Choosing remote displays feels daunting. A wrong choice impacts diagnoses. What are the absolute must-haves for these vital screens?
For remote breast reading displays, prioritize high resolution (5MP minimum) and strict DICOM compliance. High brightness, excellent contrast, and reliable, consistent calibration are absolutely essential for diagnostic confidence and accuracy.
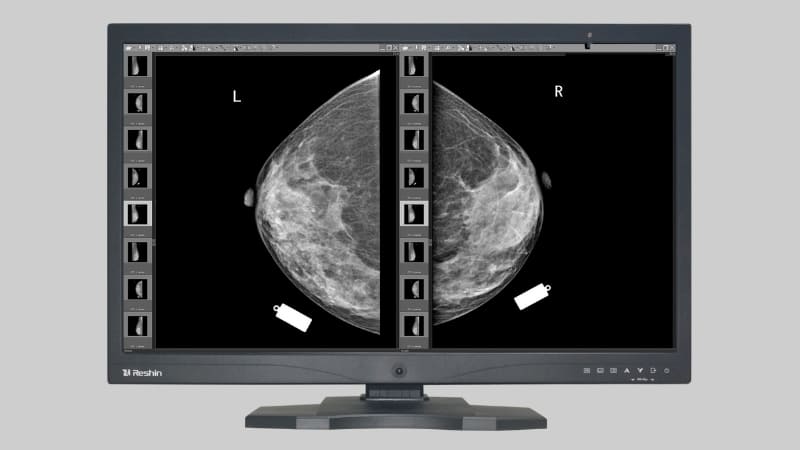
As a manufacturer, I’ve seen how critical the right display is, especially in a demanding field like breast radiology. When a radiologist is working remotely, their monitor is their window to the patient’s condition. There’s no room for compromise. My first point here echoes what I said earlier, but it bears repeating with emphasis on the display choice itself: Breast radiology demands extremely high image fidelity — telework setups must never compromise on display quality. I always emphasize 5MP or higher, DICOM-calibrated monitors10 for remote reads. A 5MP monitor provides the pixel density needed to resolve those tiny microcalcifications. Anything less, and you risk them being invisible or misinterpreted.
My second point is about why specialized displays are non-negotiable11: Consumer-grade displays are not an option. Even if remote work is flexible, diagnostic accuracy isn’t — subtle microcalcifications can’t be missed. Medical displays like ours at Reshin undergo stringent quality control. They are designed for stable brightness over long periods and can accurately render many more shades of gray than a typical office monitor. This is vital for perceiving subtle density differences in breast tissue. My final key insight, from our perspective at Reshin, is this: From a display manufacturer’s view, enabling confident remote diagnosis is a responsibility. That’s why at Reshin, we focus on delivering high-brightness, high-resolution, DICOM-compliant monitors12 tailored for teleradiology environments. This means built-in calibration sensors, tools for quality assurance, and designs that support ergonomic remote workstations. We understand that a radiologist’s confidence depends on trusting the image they see.
Key Display Considerations for Remote Breast Reading
| Display Feature | Importance for Breast Imaging | Reshin’s Focus |
|---|---|---|
| Resolution (≥5MP) | Essential for visualizing microcalcifications, fine detail. | Offers a range of 5MP and higher resolution displays. |
| DICOM GSDF Calibration | Ensures accurate and consistent grayscale reproduction. | All medical displays are DICOM Part 14 compliant. |
| Brightness & Contrast | Critical for perceiving subtle density differences. | High brightness (e.g., 1000 cd/m²) and contrast ratios. |
| Stability & QA | Consistent performance over time, easy quality checks. | Built-in front sensors, QA software compatibility. |
| Viewing Angle | Consistent image quality from different viewing positions. | Wide viewing angles for flexible setups. |
Choosing the right display is a foundational step for any successful remote breast imaging program.
Conclusion
Telework can support breast radiology effectively. However, it demands strict adherence to high technical standards. Quality displays and controlled environments are key to protecting patient care.
- Learn about the accuracy of mammogram readings done remotely and the technology involved in ensuring high-quality results. ↩
- Explore this link to understand the evolution of teleradiology and its critical role during the pandemic, enhancing healthcare delivery. ↩
- Learn about the significance of medical-grade displays in remote diagnostics, crucial for accurate and reliable healthcare delivery. ↩
- Discover insights on how remote diagnosis has transformed healthcare practices, ensuring continuity and flexibility for medical professionals. ↩
- Explore this resource to understand the importance of image fidelity in breast radiology and how it impacts diagnosis. ↩
- Learn about DICOM-calibrated monitors and their critical role in ensuring accurate remote reads in radiology. ↩
- Discover how digital breast tomosynthesis enhances breast cancer detection and the technology behind it. ↩
- Understanding the significance of 5MP resolution can enhance diagnostic accuracy in breast imaging. Explore this link for detailed insights. ↩
- Lighting control is vital for accurate image interpretation. Discover how it impacts diagnostics and best practices in this article. ↩
- Explore this link to understand how high-quality monitors enhance diagnostic accuracy in breast radiology, ensuring no detail is missed. ↩
- This resource will explain the critical differences between specialized and consumer-grade displays, emphasizing their importance in medical diagnostics. ↩
- Learn about the essential features of monitors designed for teleradiology, ensuring optimal performance and accuracy for remote diagnostics. ↩



