Managing display brightness in a hospital is a constant balancing act. A screen that is too bright causes eye strain and wastes energy, while one that is too dim can obscure critical clinical details.
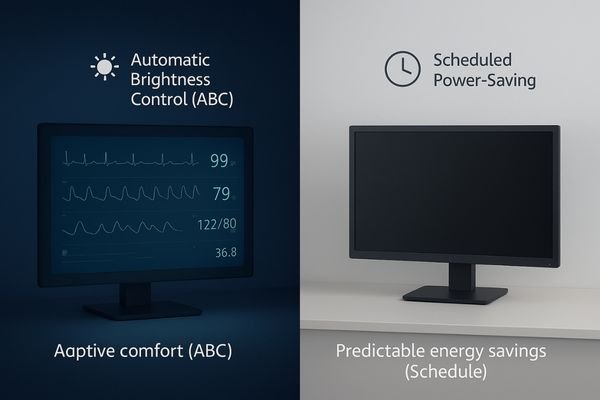
Automatic brightness control (ABC) uses ambient light sensors for real-time adaptation, while scheduled power-saving uses timers for predictable energy reduction. The optimal strategy combines both features to maximize user comfort, ensure consistent diagnostic performance, and support hospital sustainability goals.
In any clinical setting, from a brightly lit operating room to a darkened radiology reading suite, the monitor’s brightness must be appropriate for both the task and the environment. Getting this right is not just a matter of convenience; it is a critical component of diagnostic accuracy, clinical efficiency, and user well-being. Historically, managing this was a manual, often neglected, task. Today, medical-grade displays1 offer intelligent solutions: automatic brightness control2, which adapts to changing light conditions in real time, and scheduled power-saving modes, which enforce energy efficiency during idle hours. Understanding how these two technologies work, their respective benefits, and how they complement each other is essential for any healthcare institution looking to optimize its imaging infrastructure for performance, cost-effectiveness, and regulatory compliance.
Technical Principles of Brightness Management
Without intelligent controls, a display’s brightness is static, leading to eye fatigue in dim rooms and wasted energy when left on at full power. This creates both ergonomic and operational inefficiencies.
Automatic brightness control (ABC) uses ambient light sensors to dynamically adjust the backlight in real time. In contrast, scheduled power-saving is timer-based, dimming or powering down the monitor at predefined times.
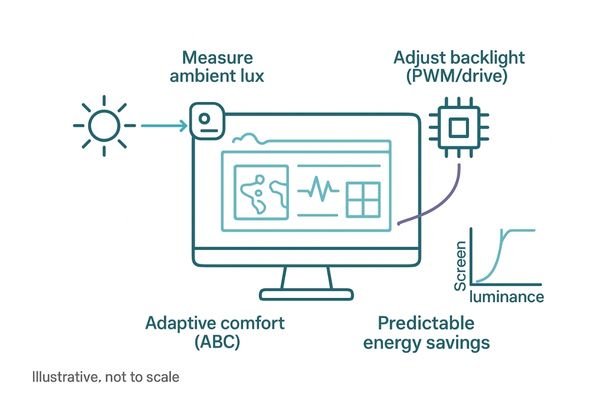
The two primary methods of intelligent brightness management operate on distinct principles. Automatic brightness control3 is a dynamic, responsive system. It relies on an integrated ambient light sensor, typically a small photodiode, that continuously measures the illumination level (in lux) of the surrounding environment. This real-time data is fed to the display’s internal controller, which then adjusts the intensity of the LED backlight accordingly. This prevents the screen from being overwhelmingly bright in a dark room and ensures it remains legible when ambient lighting changes, such as when overhead surgical lamps are switched on. In contrast, scheduled power-saving4 is a proactive, rule-based system. It functions like a simple timer, allowing administrators to define specific times when the monitor should enter a low-power standby state or shut down completely—for instance, after clinic hours or overnight on a weekend. While ABC focuses on immediate adaptation and user comfort, scheduled shutdowns guarantee predictable, measurable reductions in power consumption. A general-purpose diagnostic monitor like the MD26GA often includes both features to provide maximum flexibility.
Use Cases Across Clinical Environments
Different hospital departments have vastly different lighting conditions and workflow patterns. A single, fixed brightness setting is clinically inappropriate and operationally inefficient across these varied environments.
In bright operating rooms, ABC maintains visibility against glare. In dark reading rooms, it reduces eye strain while preserving DICOM calibration. Scheduled modes save energy across all departments during off-hours.
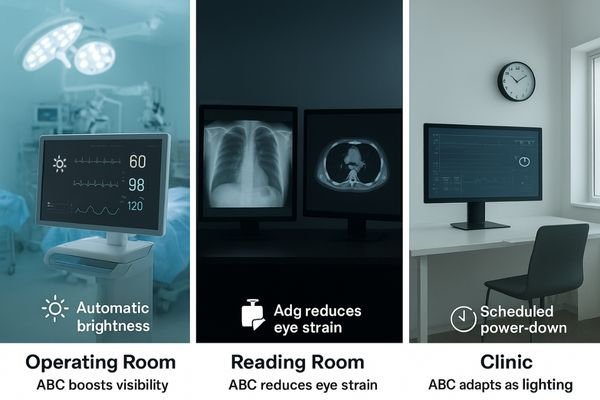
The utility of these brightness management features becomes clear when examining their application in diverse clinical settings. Each environment presents a unique challenge that a combination of ABC and scheduled modes can solve.
| Environment | Lighting Challenge | ABC Function | Scheduled Mode Function |
|---|---|---|---|
| Operating Room | Extremely high and variable ambient light (can exceed several thousand lux) from surgical lamps. | Dynamically boosts display luminance to maintain contrast and visibility against intense glare. | Powers down displays overnight when the OR is empty, reducing energy consumption. |
| Radiology Room | Very low and controlled ambient light (20–40 lux per ACR guidelines) to maximize diagnostic acuity. | Prevents eye strain by automatically reducing screen brightness to a comfortable, calibrated level. | Powers down workstations after hours, ensuring energy savings and prolonging backlight life. |
| Outpatient Clinic | Highly variable lighting as staff move between bright corridors and dimmer exam rooms. | Provides seamless adaptation, ensuring the screen is always legible without manual adjustment. | Shuts down monitors outside of a clinic’s 9-to-5 operating hours for significant energy savings. |
In radiology, where a 3MP display like the MD32C is calibrated to a specific luminance (e.g., 350 cd/m²) for DICOM GSDF compliance, ABC can gently adjust brightness for user comfort while maintaining that crucial diagnostic curve. The two functions work in concert to support clinical workflow and hospital efficiency.
Pros and Cons of Each Approach
Choosing between automatic adaptation and scheduled efficiency seems like a simple trade-off. However, deploying only one method leaves significant ergonomic and operational gaps.
ABC offers transparent, real-time convenience and reduces long-term stress on the backlight. Scheduled power-saving guarantees energy reduction but lacks adaptability. The optimal approach is to use both in tandem.
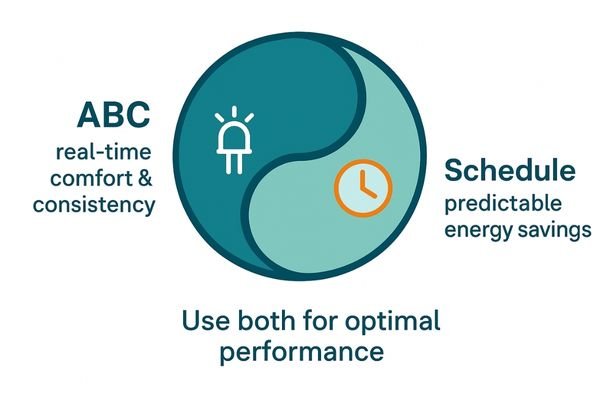
Each brightness management strategy offers distinct advantages and disadvantages. Automatic brightness control is completely transparent to the user; it adapts to the environment without requiring any manual intervention, enhancing convenience and reducing task interruptions. By ensuring the display is never unnecessarily bright, it also reduces long-term thermal and electrical stress on the LED backlight components, which can slow performance degradation and extend the monitor’s operational lifespan. Its primary drawback is that its energy savings are variable, depending entirely on ambient conditions. Scheduled power-saving1, on the other hand, delivers absolute and verifiable energy savings by cutting power consumption to near-zero levels during designated idle periods. Its weakness is its rigidity; it cannot adapt to real-time workflow changes. The most effective strategy is therefore not to choose one over the other but to combine them. A multi-modality display like the MD85CA benefits from using ABC for real-time adaptation during clinical use, ensuring consistent performance, while a scheduled shutdown mode handles routine efficiency overnight. This dual approach maximizes display longevity, lowers operational costs, and maintains peak imaging performance.
Ambient Adaptation and Nighttime Operation
Poorly managed brightness can compromise patient care. An image that is too dim can hide details, while abrupt changes in luminance can disrupt a clinician’s concentration.
Properly tuned ABC prevents loss of detail as lighting changes, while scheduled modes must allow for quick overrides to support emergency nighttime work without compromising hospital sustainability goals.

Effective ambient adaptation5 is a key contributor to clinical safety. ABC ensures that critical image details on a high-resolution display like the MD120C remain visible even as ambient lighting conditions fluctuate. However, the system must be carefully tuned to avoid sudden, jarring shifts in brightness, as studies indicate that the human eye can require several minutes to fully re-adapt after a significant mismatch between display and ambient luminance. This prevents visual fatigue and allows the clinician to maintain focus. The safety implications of scheduled power-saving are different. While shutting down idle equipment aligns with hospital safety and sustainability initiatives by reducing fire risk and energy waste, the system must be flexible. It must include a simple and rapid override mechanism. An emergency surgery or an urgent overnight radiological review cannot be delayed because a monitor has entered a locked power-saving state. When properly implemented, these two features complement each other: ABC ensures continuous clinical visibility during active use, while scheduled shutdowns provide predictable efficiency without hindering a hospital’s 24/7 readiness for urgent patient care.
Fail-Safe Design and Recovery Mechanisms
A smart feature is only useful if it is reliable. A brightness control that fails or a power-saving mode that cannot be overridden can disrupt clinical workflow at a critical moment.
Medical-grade displays must include fail-safes, such as reverting to a default brightness if a sensor fails and providing a manual override for scheduled power-saving modes to ensure uninterrupted clinical access.
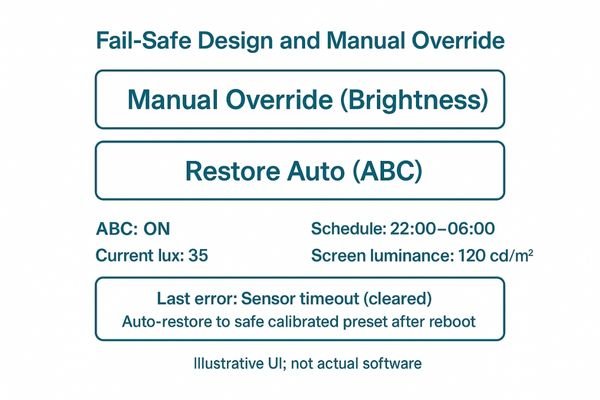
The design of any automated system in a medical environment must prioritize reliability and graceful failure. For automatic brightness control6, a key fail-safe mechanism7 involves the display’s firmware. If the ambient light sensor were to fail or provide an erroneous reading, a well-designed monitor like the MD33G will not simply go dark. Instead, it should revert to a pre-set, safe default luminance level—one that is bright enough for general clinical use—and notify the user or IT administrator of the sensor fault. This ensures the display remains usable until the issue can be addressed. For scheduled power-saving modes, the critical recovery mechanism is the manual override. Staff must be able to wake a monitor instantly and intuitively with a simple mouse movement, keyboard press, or button push, regardless of the schedule. This is essential for emergency situations or unexpected after-hours work. Furthermore, remote management tools should allow administrators to temporarily disable or adjust schedules for specific rooms or entire departments, providing another layer of operational flexibility. These fail-safes transform smart features from potential points of failure into robust, trustworthy tools.
Regulatory and Ergonomic Guidelines
Hospitals do not operate in a vacuum. Equipment must comply with stringent regulatory standards and support established ergonomic best practices to ensure both patient safety and staff well-being.
IEC 60601 mandates essential performance, while FDA and DICOM standards govern diagnostic displays. ABC helps meet ergonomic guidelines by automatically adapting brightness to recommended ambient light levels.
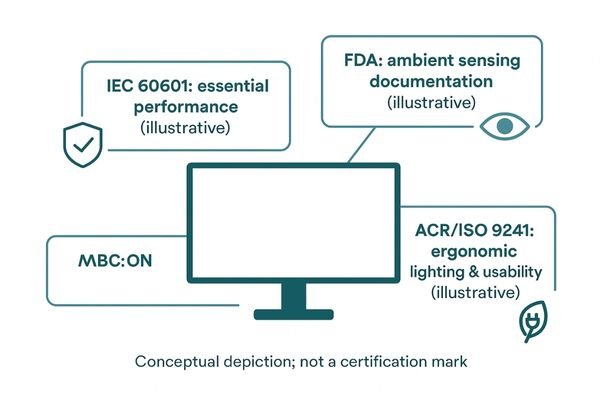
Regulatory and ergonomic standards provide a clear framework for the design and use of medical displays. The international standard IEC 60601-1 demands that a device maintains its "essential performance" for safety, which includes providing a clear, usable image. FDA guidance for diagnostic monitors often requires documentation of features like ambient light sensing8, acknowledging its role in maintaining consistent image quality. For diagnostic imaging, compliance with the DICOM Part 14 Grayscale Standard Display Function (GSDF)9 is non-negotiable. ABC supports this by helping maintain perceptual consistency as viewing conditions change. Ergonomic guidelines, such as the American College of Radiology’s (ACR) recommendation for low ambient light (20–40 lux) in reading rooms, make ABC particularly valuable. A dual-screen diagnostic display like the MD45C can automatically adjust its brightness to match these dimmed environments, reducing eye strain and helping the facility adhere to best practices. Simultaneously, scheduled power-saving supports hospitals’ growing "green" initiatives and aligns with ISO ergonomic standards that emphasize both user comfort and environmental sustainability by reducing idle power consumption. A display like the MD52G is a great example of this principle in action. Even a dual-head color display like the MD46C benefits from these smart features for longevity and user comfort.
Conclusion
Combining automatic brightness control for real-time adaptation with scheduled power-saving for off-hour efficiency provides a comprehensive solution for managing modern medical displays.
👉 For tailored advice on implementing advanced display management solutions, contact Martin at martin@reshinmonitors.com.
-
Learn about medical-grade displays to see how they improve imaging infrastructure and ensure compliance in healthcare environments. ↩ ↩
-
Explore this link to understand how automatic brightness control enhances diagnostic accuracy and user comfort in clinical settings. ↩
-
Explore this link to understand how Automatic brightness control enhances user experience by adapting to ambient light. ↩
-
Discover the advantages of scheduled power-saving, including energy efficiency and cost savings for your devices. ↩
-
Understanding ambient adaptation can enhance clinical safety and improve patient care by ensuring optimal visibility. ↩
-
Understanding automatic brightness control can enhance your knowledge of display technology in medical environments. ↩
-
Exploring fail-safe mechanisms will provide insights into how medical devices ensure reliability and safety. ↩
-
Exploring ambient light sensing reveals its importance in maintaining consistent image quality, crucial for accurate diagnostics. ↩
-
Understanding GSDF is crucial for ensuring compliance in diagnostic imaging, enhancing image quality and safety. ↩



