Choosing the right mammography monitor setup is a critical decision in breast imaging. The wrong choice can reduce workflow efficiency and compromise the subtle detections that are vital for early breast cancer diagnosis.
Dual 5MP is proven and precise; a single 12MP is faster and more flexible. Choose by workflow: if bilateral symmetry, priors, and DBT must sit side-by-side, 12MP reduces motion and bezel artifacts; if fixed dual heads are standard, dual 5MP stays robust. In all cases, demand DICOM Part 14, luminance stabilization, and acceptance QA.
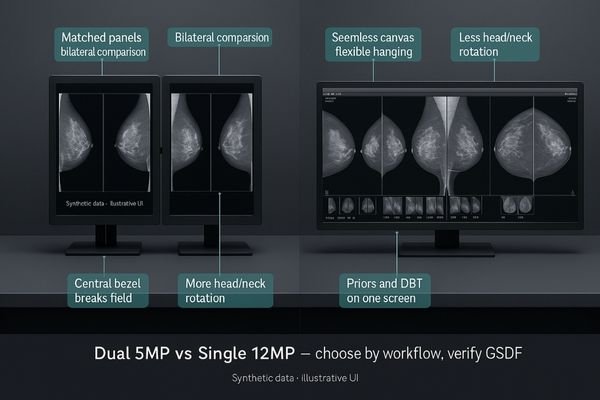
The debate between dual 5MP mammography monitors1 and a single 12MP display is fundamentally about workflow optimization and ergonomic efficiency. The traditional dual setup provides a familiar, dedicated screen for each breast, excelling at direct left-right comparisons. However, it introduces a physical bezel that breaks the visual field and requires more head and neck movement when cross-referencing priors. In contrast, a single 12MP display2 like the MD120C offers a seamless, unified canvas with higher pixel density. This allows flexible hanging protocols where current and prior images can be arranged side-by-side without obstruction, potentially speeding navigation and reducing fatigue. The decision comes down to balancing the robustness of a dual-head workflow against the consolidated efficiency and flexibility of a large, single-screen solution. Regardless of the choice, the foundations remain non-negotiable: verifiable DICOM conformance and stable luminance are essential for diagnostic confidence.
Diagnostic Confidence and Workflow with Mammography Monitors
Selecting the right monitor configuration is a critical decision. This choice directly shapes a radiologist’s daily workflow, impacting both diagnostic confidence and physical comfort during long reading sessions.
Dual 5MP monitors offer a proven, matched-panel approach for bilateral comparison, while a single 12MP streamlines multi-image layouts. The optimal choice depends on whether the workflow prioritizes fixed symmetry or flexible navigation.

The established standard for full-field digital mammography (FFDM) has long been a pair of 5MP monitors3. This setup, often using monitors like the MD52G, ensures each breast image is presented on a dedicated, factory-matched panel, providing consistency in grayscale and white point for left-right comparisons. This familiarity offers a robust and predictable workflow that many radiologists rely on. However, the emergence of single 12MP mammography monitors4 presents a compelling alternative rooted in efficiency. By consolidating the workspace onto a single, uninterrupted surface, the central bezel disappears, reducing the visual gap and minimizing head rotation. This unified canvas is particularly advantageous for cases involving multiple priors or digital breast tomosynthesis (DBT) slices, enabling more fluid navigation. The decision is not about which is absolutely better, but which best aligns with the team’s hanging protocols and ergonomic preferences.
| Feature Comparison | Dual 5MP Monitors | Single 12MP Monitor |
|---|---|---|
| Bilateral Comparison | Ideal; two physically separate but matched panels. | Excellent; seamless canvas with no central bezel. |
| Ergonomics | More head/neck rotation to view both screens. | Less head/neck rotation; centralized viewing. |
| Footprint | Larger desk footprint, more cables. | Smaller footprint, simplified cabling. |
| Flexibility | Fixed dual-view layout. | Highly flexible; supports various multi-image layouts. |
DICOM Part 14 Compliance and Luminance Stabilization in Mammography
In mammography, even the slightest deviation in grayscale can hide a critical finding. Relying on factory specifications alone is insufficient; performance must be actively managed and verified over time.
True diagnostic confidence in mammography requires monitors with active luminance stabilization and verifiable DICOM conformance. Rigorous acceptance QA and routine calibration are essential to ensure subtle micro-calcifications remain visible long-term.

The visibility of micro-calcifications and subtle distortions is directly tied to the display’s ability to follow the DICOM GSDF curve5 at a high, stable luminance. Specifications are only a snapshot in time. Without active management, panel aging and thermal stress cause luminance and color temperature drift, potentially masking faint signals. High-performance mammography monitors integrate closed-loop luminance stabilization6, where an internal sensor continuously adjusts the backlight to maintain constant brightness. An ambient light sensor further helps preserve perceptual consistency as room lighting changes. Acceptance QA must validate this at installation, and automated monthly checks with quarterly calibrations ensure ongoing stability. This disciplined approach ensures display performance is a known constant, not a hidden risk.
DBT and Prior Comparison on High-Resolution Mammography Displays
Reading DBT and comparing multiple priors demand a flexible display workspace. A rigid screen setup can slow down navigation and make it difficult to arrange images effectively.
Single high-resolution displays excel at DBT and prior review by enabling flexible, side-by-side hanging protocols on one screen. This ensures each window maintains GSDF consistency, streamlining complex case navigation effectively.
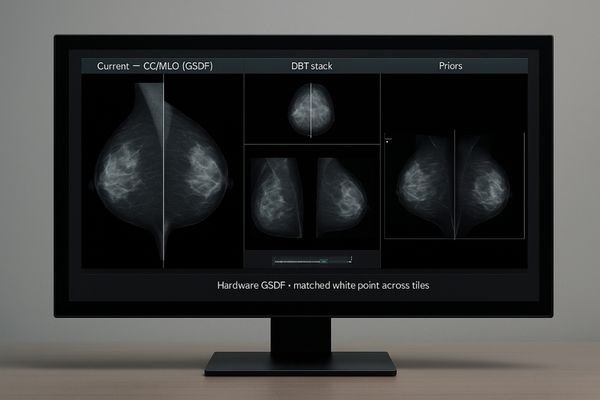
Digital breast tomosynthesis (DBT)7 generates hundreds of slices that must be reviewed alongside 2D synthesized images and historical priors. This complex dataset benefits enormously from a large, flexible display. A multi-modality monitor8 like the MD85CA leverages its resolution to create multiple virtual screens within one panel. Radiologists can arrange current CC/MLO pairs next to priors, or view a magnified region alongside the DBT cine loop. The display software must ensure each window independently maintains DICOM compliance, luminance, and white point stability. This prevents visual discrepancies when comparing a new finding to a subtle density on a prior exam. While dual 5MP setups can achieve this with synchronized protocols, the single-screen approach offers greater fluidity and reduces cognitive load.
Total Cost of Ownership and Room Design for Mammography Monitors
The cost of a display extends far beyond its initial purchase price. Factors like energy consumption, desk space, and the manpower required for quality assurance all contribute to the total cost of ownership (TCO).
A single 12MP monitor can lower TCO by reducing footprint, power consumption, and heat output compared to a dual-5MP setup. This streamlined approach also simplifies cabling and centralizes quality assurance tasks.
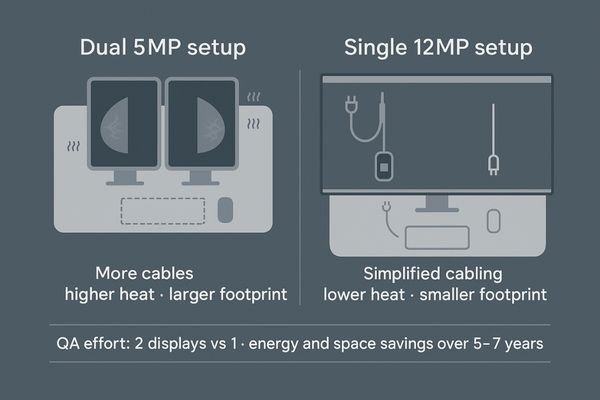
A traditional dual 5MP setup involves two separate power supplies, video cables, and physical units that generate heat and occupy more desk space. A single 12MP monitor9 consolidates this into one unit, leading to a smaller footprint, reduced power use, and less heat in the reading room. Maintenance and QA are also simplified—calibrating and managing one monitor10 is inherently more efficient than two. Over a five-to-seven-year lifespan, savings in power, space, and labor can be significant. Regardless of setup, room design must support it. Standardized lighting and ergonomic placement ensure the investment in high-quality displays is not undermined by inconsistent conditions.
Pixel Pitch and 1:1 Mapping for Micro-calcification Detection
The smallest details determine outcomes in mammography. If display pixels are not perfectly matched to image data, subtle but critical findings like micro-calcifications can be softened or lost.
To ensure micro-calcifications are visible, the display must support 1:1 pixel mapping without scaling. A small pixel pitch, combined with luminance stabilization and uniformity correction, is essential for preserving the integrity of these tiny signals.
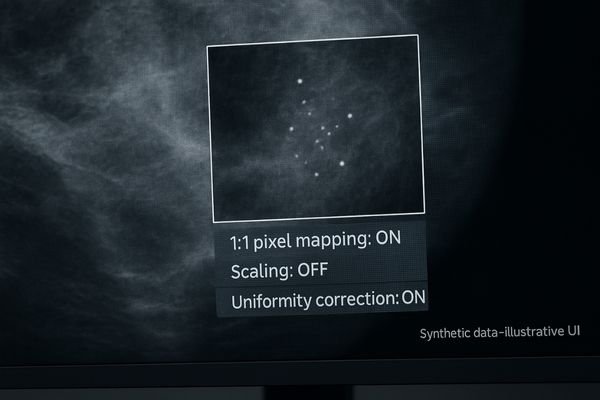
The diagnostic utility of a mammography monitor depends on resolving the finest details. Central to this is the relationship between pixel pitch and image data. To avoid image degradation, 1:1 pixel mapping is mandatory—each image pixel must map to one display pixel, without interpolation that could blur edges. This is crucial for visualizing micro-calcifications, which may be only a few pixels in size. A panel with small pixel pitch11 offers higher pixel density, producing a sharper image. Yet pixel pitch alone is not enough. Uniform luminance across the entire screen is critical, as a dark spot could easily obscure low-contrast findings. Rigorous acceptance QA must validate proper 1:1 mapping and uniform brightness corner to corner.
| Technical Factor | Why It’s Critical for Mammography |
|---|---|
| 1:1 Pixel Mapping | Prevents scaling artifacts that can soften or blur micro-calcifications. |
| Luminance Stabilization | Ensures that low-contrast signals are consistently visible throughout the day. |
| Uniformity Correction | Prevents dark or bright spots on the screen from masking pathology. |
| Low Black Level | Improves contrast ratio, making subtle density differences more apparent. |
Ergonomic Reading Environments with AR Glass and Ambient Light Control
A radiologist’s ability to detect subtle abnormalities depends on both image quality and human factors. Fatigue and distraction from poor ergonomics or glare can lead to missed findings.
An ergonomic reading environment combines AR-bonded glass and controlled lighting to minimize glare and fatigue. The choice between single and dual monitors should consider the impact on head and neck movement.
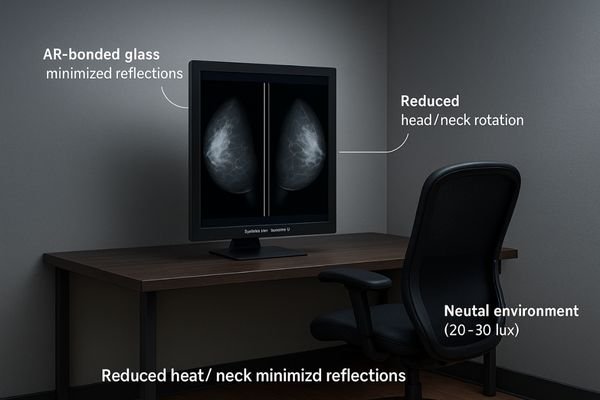
The interface between radiologist and display is a critical factor in diagnostic performance. Glare from lighting can create reflections that wash out contrast and force higher brightness settings. High-quality mammography monitors12 mitigate this with AR-coated, optically bonded glass that eliminates internal reflections and maximizes contrast. Ergonomics also matters. A single 12MP monitor reduces head and neck rotation compared to dual displays, lowering musculoskeletal strain13 during long sessions. Conversely, a dual 5MP setup may feel more familiar and provides distinct separation of views. The workstation—chair, desk height, and VESA mount placement—must support the chosen configuration. By controlling environment and ergonomics, radiologists can focus fully on the image.
Conclusion
Ultimately, whether using a dual 5MP or single 12MP setup, diagnostic success depends on verifiable DICOM performance, active stabilization, and an ergonomic workflow that minimizes fatigue and distraction, ensuring accurate and confident diagnoses across the entire enterprise. 🔎
👉 For professional advice and Reshin’s diagnostic display solutions, contact martin@reshinmonitors.com.
-
Explore the benefits of dual 5MP monitors for mammography, including workflow optimization and ergonomic efficiency. ↩
-
Discover how a single 12MP display enhances mammography workflow with seamless image viewing and reduced fatigue. ↩
-
Explore this link to understand how 5MP monitors enhance image quality and workflow in mammography. ↩
-
Discover the advantages of 12MP monitors and how they can streamline your mammography process. ↩
-
Understanding the DICOM GSDF curve is crucial for ensuring optimal display performance in medical imaging, enhancing diagnostic accuracy. ↩
-
Exploring closed-loop luminance stabilization can reveal how it maintains consistent brightness, crucial for detecting subtle signals in mammography. ↩
-
Understanding DBT is crucial for grasping its impact on breast cancer detection and diagnosis. ↩
-
Exploring the advantages of multi-modality monitors can enhance your knowledge of modern imaging technologies. ↩
-
Explore the advantages of a 12MP monitor, including space-saving and efficiency, to enhance your workspace. ↩
-
Learn best practices for calibrating a single monitor to ensure consistent quality and performance in your setup. ↩
-
Understanding pixel pitch is essential for optimizing image quality in mammography, ensuring accurate diagnostics. ↩
-
Explore how high-quality monitors enhance diagnostic accuracy and reduce glare, crucial for effective radiology. ↩
-
Learn about strategies to minimize strain and improve comfort for radiologists during extended work hours. ↩



