[========]
Purchasing medical displays based on consumer-centric specs can be a costly mistake. Believing common myths can lead to acquiring equipment that fails to meet clinical, safety, or regulatory standards.
Most “gotchas” come from treating resolution as quality. In practice, safety certifications, AR-bonded optics, DICOM Part 14 with stabilized luminance, ambient compensation, and robust OR connectivity decide clinical truth. Pick the right size and I/O for the workflow, keep GSDF verified on a schedule, and wide gamut only when the entire chain preserves it.
In medical imaging, what you see directly impacts patient outcomes. Yet, the market is filled with displays that use consumer-friendly terms that can be misleading in a clinical context. Distinguishing between a true medical-grade display1 and a high-resolution office monitor is critical for ensuring diagnostic accuracy2, surgical precision, and patient safety. This discussion will dissect seven common misconceptions about medical displays, providing the clarity needed to make informed procurement decisions that align with the rigorous demands of modern healthcare.
4K = medical-grade? Why certifications and optics matter
Many assume that any 4K display is suitable for medical use. This overlooks the strict safety and performance standards that define a true medical-grade device, leading to compliance risks and poor image quality.
A display’s "medical-grade" status is determined by IEC 60601-1 certification, DICOM conformance, and specialized optics, not just its 4K pixel count. Without these, high resolution offers no guarantee of clinical reliability.
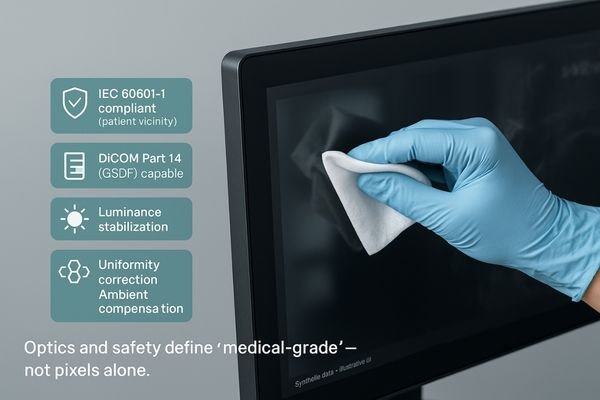
The term "medical-grade" is a system-level property, not just a resolution badge. While a 4K resolution provides a detailed canvas, it is meaningless without the foundational layers of safety and image fidelity. For a surgical display, this begins with IEC 60601-1 certification for electrical safety, which is essential for any equipment used in the patient vicinity. It also demands physical robustness, including sealed front panels that can be wiped down for infection control and optically bonded, anti-reflection (AR) glass that maintains contrast and clarity under bright OR lights. For diagnostic displays, being medical-grade3 means strict, verifiable adherence to the DICOM Part 14 GSDF standard4. Features like built-in luminance stabilization, uniformity correction, and ambient light compensation work together to ensure that pixel data is rendered faithfully and consistently. A premium diagnostic monitor like the MD46C incorporates these features to deliver trustworthy images. Without these critical elements, a 4K monitor is simply a high-resolution screen, not a reliable medical instrument.
More nits, better diagnosis—really?
There is a common belief that higher brightness always results in a better image. This can lead to a focus on maximum nit values, ignoring the more important factors that contribute to diagnostic visibility.
Excessive brightness without proper GSDF conformance can wash out contrast and cause eye fatigue. Clinicians need calibrated, stable luminance within a controlled ambient environment to perceive subtle diagnostic cues consistently.
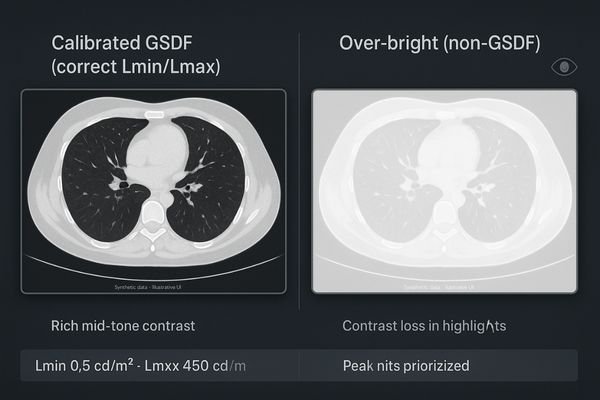
Brightness improves visibility only when it is controlled. Chasing a higher number of "nits" (a measure of luminance) is a distraction from what truly matters for diagnostics. An excessively bright screen that does not conform to the DICOM GSDF curve5 can actually harm image quality by compressing contrast in bright areas and causing significant eye fatigue for the radiologist. What clinicians truly need is calibrated and stable luminance6. This means having a well-defined Lmin (black level) and Lmax (peak white) that are consistent with the GSDF standard for a given ambient light level. Furthermore, the monitor must achieve this stable luminance rapidly after being powered on and maintain it throughout the day. High-end displays designed for demanding modalities, like the MD52G for mammography, prioritize luminance stabilization and uniformity over raw peak brightness. This consistency ensures that subtle cues, like micro-calcifications or soft-tissue variations, are just as perceptible at the end of a long shift as they are at the beginning.
Set DICOM once and forget it” in real clinics?
A frequent misconception is that a monitor’s factory DICOM calibration is permanent. This "set and forget" mindset ignores the inevitable performance degradation that occurs over time, creating a compliance risk.
DICOM conformance is not permanent; it drifts due to component aging and environmental changes. Regular, scheduled QA and displays with automated stabilization are essential to maintain compliance over the long term.

A one-time factory calibration is merely a starting point. The performance of any display drifts over time; the phosphors or LEDs that produce light dim with age, internal sensors can deviate, and the electronics are stressed by thousands of power-on/off and cleaning cycles. Believing that a monitor will remain in DICOM conformance without ongoing verification is a dangerous assumption. In a real clinical environment, performance must be actively managed. This is why a robust Quality Assurance (QA) program7 is essential. Medical displays must be designed to support this workflow, offering features that facilitate quick and accurate QA checks for the physics team. More advanced monitors like the MD32C integrate closed-loop luminance stabilization8 and automated GSDF monitoring. These systems constantly check their own output and make micro-adjustments to counteract drift, ensuring the display remains within spec. This active management, not a one-time setting, is what guarantees reliable diagnostic quality.
BT.709 vs BT.2020: Do surgeons actually benefit?
The technical difference between color gamuts like BT.709 and BT.2020 can seem abstract. This leads to skepticism about whether the wider gamut of BT.2020 offers any tangible benefit in the operating room.
In endoscopy, BT.2020 is beneficial when the entire imaging chain supports it. It preserves saturated reds and greens without clipping, but the benefit is lost if any component collapses the signal back to BT.709.
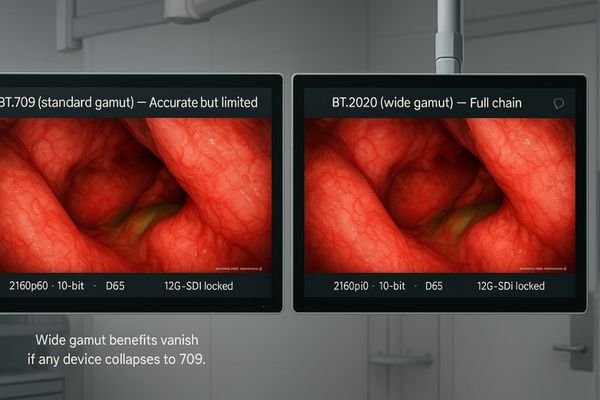
Surgeons absolutely can benefit from the wider BT.2020 color gamut[^91], but only under specific conditions. This is not about making colors "prettier"; it is about preserving diagnostic information. In procedures like endoscopy and Minimally Invasive Surgery (MIS)9, modern cameras and light sources can capture highly saturated reds and greens that fall outside the boundaries of the standard BT.709 color space. When displayed on a BT.709 monitor, this extra color information is "clipped," resulting in flat, undifferentiated patches of color where subtle textural details should be. A BT.2020-capable monitor like the MS322PB, when part of a complete wide-gamut chain, can faithfully render these saturated tones, preventing clipping and inaccurate hue shifts. However, this benefit evaporates if any single link in the chain—from the camera to the video processor to the monitor—collapses the signal back to BT.709. Therefore, the decision to invest in BT.2020 must be an end-to-end system decision.
HDMI-only OR integration is fine—right?
Many assume that HDMI, being a common standard, is sufficient for OR video integration. This ignores the unique environmental and reliability challenges of the operating room, where consumer-grade connections can be a weak link.
HDMI is suitable for short runs, but 12G-SDI is the robust choice for ORs. It offers locking connectors and superior noise immunity over long distances, preventing signal drops that disrupt surgical workflow.

While HDMI is a capable interface that is perfect for connecting devices on a mobile cart or over short distances, it is not the ideal solution for fixed OR integration. Operating rooms are electromagnetically noisy environments, and video signals often need to travel long distances from a equipment boom to a wall display. The non-locking connectors of HDMI can become dislodged by incidental contact, causing a sudden loss of video at a critical moment. The professional standard for this application is 12G-SDI. It uses robust, locking BNC connectors10 and coaxial cable that provides excellent immunity to RF interference over long runs, ensuring a stable 4K 60Hz signal. A well-designed surgical display like the MS321PB will offer a flexible array of inputs, including 12G-SDI, DisplayPort, and HDMI. This multi-I/O approach allows for robust primary connections via SDI while retaining compatibility with other sources, reducing the need for signal converters and minimizing potential points of failure.
Bigger screens always beat smaller ones
There is a simple intuition that a larger screen must be better. This can lead to purchasing oversized monitors that are ergonomically unsuited for the specific clinical task, potentially increasing fatigue and inefficiency.
The optimal screen size is determined by viewing distance and task, not an ideology of "bigger is better." The right size minimizes head movement for primary tasks while ensuring legibility for shared information.
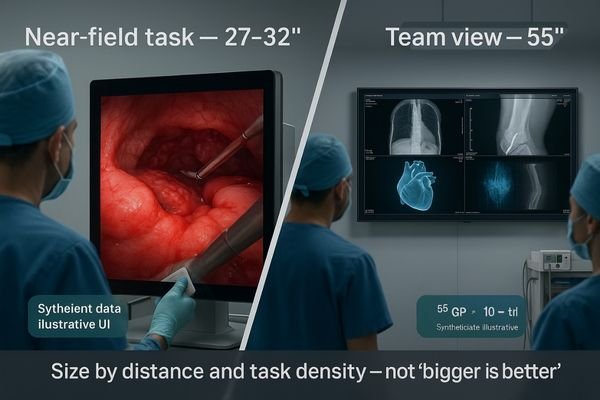
The idea that "bigger is always better" is one of the most pervasive but incorrect assumptions in display procurement. Screen size must be chosen based on ergonomics and the specific workflow. A surgeon performing a procedure needs key information within their immediate field of view to minimize head and eye movement, which can cause fatigue and distraction. For these near-field tasks, a 27-inch display11 like the MS270P is often ideal. A slightly larger 32-inch screen placed on an endoscopy tower works well for balancing a clear primary view with space for secondary picture-in-picture (PIP) information. In contrast, a large 55-inch wall display12 like the MS550P is not meant for a single user; its purpose is to distribute shared situational awareness to the entire team in a hybrid OR or training environment, where it can be viewed clearly from several meters away. Choosing the right size for the viewing distance and task density is far more important than simply choosing the largest screen available.
Any office monitor can serve as a PACS display
The high resolution and image quality of modern office monitors lead many to believe they are adequate for PACS reading. This overlooks the essential quality control features that underpin diagnostic confidence and legal defensibility.
Office monitors lack the critical guardrails of a true PACS display, such as DICOM Part 14 conformance, luminance stabilization, and uniformity correction. Using one undermines diagnostic confidence and medico-legal traceability.

This is perhaps the most dangerous misconception. While a high-end office monitor may look sharp and vibrant when displaying photographs, it is entirely unsuited for primary diagnostic reading. A PACS display13 is a scientific instrument. Its value comes not from its peak brightness or color gamut, but from its ability to render images with verifiable consistency. This is achieved through a suite of medical-grade controls14 that office monitors simply do not have. These include automated tracking of the DICOM GSDF curve, real-time luminance stabilization to compensate for warm-up and aging, ambient light compensation to ensure consistent perception in different reading environments, and sophisticated uniformity correction to ensure a lesion looks the same at the edge of the screen as it does in the center. A monitor like the MD120C is built from the ground up with these features to provide the unwavering consistency that radiologists need to make confident diagnoses and to ensure the images are medico-legally defensible.
Conclusion
True clinical value comes from certified, stable, and workflow-appropriate displays, not just from high resolution or brightness figures found on a consumer-focused spec sheet. 🩺
👉 For professional guidance and Reshin medical-grade display solutions, contact martin@reshinmonitors.com.
-
Understanding the differences can significantly impact diagnostic accuracy and patient safety. ↩
-
Exploring this topic can provide insights into the importance of precise imaging for effective treatment. ↩
-
Understanding ‘medical-grade’ is crucial for ensuring safety and efficacy in medical devices. ↩
-
Exploring the DICOM standard helps ensure compliance and quality in diagnostic imaging. ↩
-
Exploring the DICOM GSDF curve will enhance your knowledge of image quality standards in radiology. ↩
-
Understanding calibrated and stable luminance is crucial for ensuring optimal image quality in medical diagnostics. ↩
-
Understanding QA programs is crucial for maintaining display performance and ensuring diagnostic accuracy in clinical settings. ↩
-
Exploring this technology reveals how it enhances display reliability and accuracy, vital for effective medical diagnostics. ↩
-
Learn about the advantages of MIS and how modern imaging improves surgical outcomes. ↩
-
Learn why locking BNC connectors are essential for secure video connections, especially in critical environments. ↩
-
Explore how a 27-inch display can enhance surgical precision and reduce fatigue for medical professionals. ↩
-
Learn about the advantages of a 55-inch wall display for team collaboration and situational awareness in hybrid ORs. ↩
-
Understanding PACS displays is crucial for anyone in the medical imaging field, as they are essential for accurate diagnostics. ↩
-
Exploring medical-grade controls will provide insights into the technology that ensures image consistency and reliability in diagnostics. ↩



