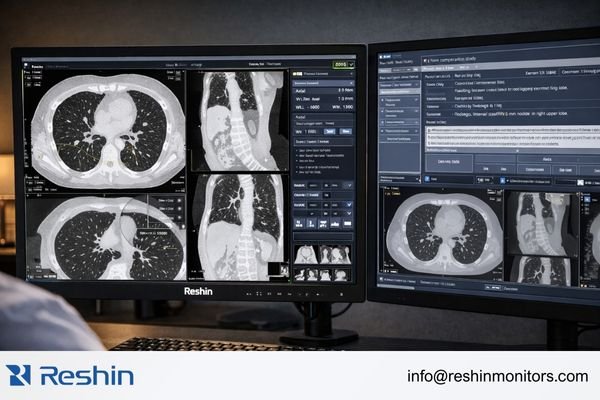
Lung-screening programs vary significantly in imaging modality, workflow design, and presentation assumptions—creating real differences in how radiology monitors should be selected, calibrated, and standardized across clinical sites.
Different lung-screening systems—from LDCT programs to AI-assisted workflows—place unique demands on radiology monitors, particularly regarding grayscale stability, overlay legibility, and consistent luminance behavior across extended reading sessions.

Many lung-screening deployments underperform not because the monitors are “bad,” but because the imaging platform’s presentation model (how it maps grayscale, assumes calibration, and renders overlays) is not aligned with the monitor’s calibrated behavior in the real reading environment. An LDCT screening program optimized for nodule detection has different display needs than a population chest X-ray workflow, and both differ from AI-augmented screening systems that layer heatmaps and probability overlays on top of anatomy. The practical challenge is matching luminance stability, grayscale mapping consistency1, and overlay handling to actual reading behavior—not just comparing generic specifications.
From an engineering perspective, the most common failure mode is variability: the same borderline finding looks slightly different across workstations or across time during long reading sessions. When calibration assumptions, grayscale response, and overlay rendering are not standardized, readers may compensate with extra window/level adjustments, inconsistent thresholds, or workflow workarounds—reducing confidence and weakening screening program consistency.
What counts as a lung-screening system in radiology?
Modern lung-screening encompasses multiple modalities and workflow designs, each creating distinct requirements for display technology and calibration approaches.
A lung-screening system can range from structured LDCT programs focused on nodule tracking to AI-assisted multi-modality workflows that integrate triage overlays, structured reporting, and automated measurements across different imaging platforms.
In practice, lung-screening systems usually fall into a few recognizable categories that influence monitor requirements:
LDCT-Based Screening Programs
Low-dose CT (LDCT) screening systems are built around thin-slice review protocols and longitudinal nodule tracking, requiring sustained attention to subtle low-contrast findings such as small pulmonary nodules and faint ground-glass change. These programs often use standardized reading protocols with fixed series presentation, defined comparison layouts for current and prior studies, and structured reporting templates. The reading pattern emphasizes detailed grayscale perception over extended sessions, making stable calibrated luminance and a predictable grayscale response especially important for consistent interpretation across many cases.
Population-Based Chest X-ray Screening
Chest X-ray screening2 workflows, common in occupational health and large population screening programs, emphasize whole-field anatomical assessment and rapid throughput. Readers evaluate large anatomical regions holistically, so full-panel uniformity and consistent grayscale mapping across the entire image area become critical. Compared with LDCT workflows, X-ray screening may involve fewer prior comparisons but higher volume, increasing the importance of visual comfort, stable presentation, and predictable tone response without frequent manual compensation.
Why does high brightness matter in lung screening?
High brightness capability becomes significant when ambient lighting conditions vary and readers must maintain consistent perception across high-volume, repetitive screening cases.
High brightness primarily improves perceived contrast under suboptimal ambient lighting and reduces visual strain during extended reading sessions, but the more critical benefit is maintaining stable calibrated luminance that prevents interpretation variability across workstations.
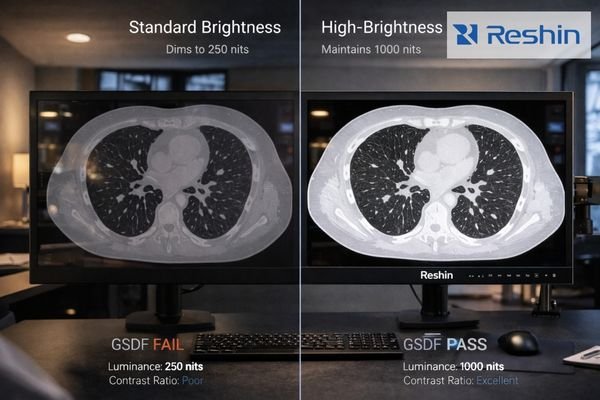
High brightness matters most when the reading environment is not a controlled dark room—common in busy radiology departments, shared reading spaces, and daytime operations. Higher luminance3 can help preserve perceived contrast under ambient light and reduce the tendency to over-adjust window/level simply to fight glare. This is particularly relevant when evaluating subtle findings near the threshold of visibility, such as faint ground-glass patterns or small nodules that require stable visual adaptation.
The larger impact is consistency. Screening requires repetitive decisions across many cases; if luminance drifts over time, or if calibrated behavior differs across workstations, the same borderline finding can look slightly different—introducing avoidable variability. For screening programs that span multiple rooms or sites, stable calibrated luminance and repeatable grayscale behavior support program-level standardization, improving reader confidence and reducing workflow friction.
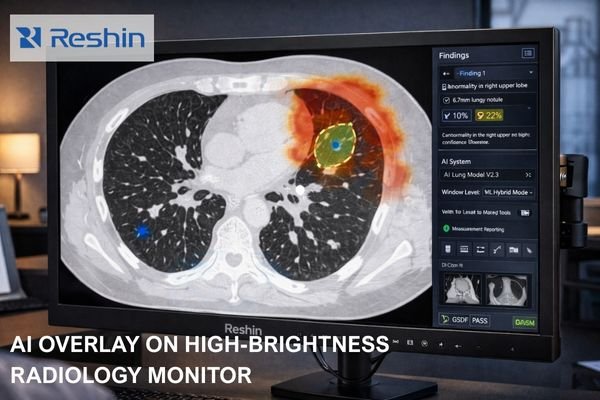
How do screening platforms differ in grayscale mapping and overlays?
Screening platforms handle pixel presentation differently based on their assumptions about display calibration, default settings, and overlay rendering priorities.
Different lung-screening platforms present the same pixel data through varying approaches to DICOM GSDF calibration, LUT management, and overlay rendering, which can significantly alter how subtle findings and AI-generated overlays appear across different systems.
| Platform Type | Grayscale Approach | Overlay Method | Monitor Requirements |
|---|---|---|---|
| LDCT Diagnostic Systems | Monitor-side DICOM GSDF4 calibration with controlled grayscale response | Minimal overlays, measurement tools emphasized | Stable grayscale response, consistent calibrated luminance |
| AI-Assisted Screening | Application-managed LUT (look-up table) behavior tuned to overlays | Heatmaps, contours, probability overlays | Consistent contrast handling, overlay legibility across window/level |
| Population X-ray Systems | Simplified calibration practices with operator presets | Basic annotations, batch workflow indicators | Full-panel uniformity, reliable grayscale mapping across the image area |
Key differences often come down to assumptions. Some diagnostic-oriented systems expect the display to behave predictably under DICOM GSDF (Grayscale Standard Display Function), while other platforms depend more heavily on application-side LUTs and user-adjustable presets. In LDCT workflows, small shifts in grayscale response can change how faint density transitions appear—affecting confidence when distinguishing subtle patterns. When AI components are integrated, overlays (heatmaps, contours, probability tags, and automated measurements) must remain readable across window settings and must not mask anatomy; this increases the importance of stable luminance behavior and consistent contrast handling at higher brightness levels.
What monitor characteristics should match LDCT vs chest X-ray screening?
Different screening modalities create distinct demands for resolution, uniformity, and calibration behavior that should drive monitor selection decisions.
LDCT screening prioritizes sustained grayscale stability and multi-series layout capability, while chest X-ray screening emphasizes full-panel uniformity and consistent grayscale mapping across large anatomical fields.
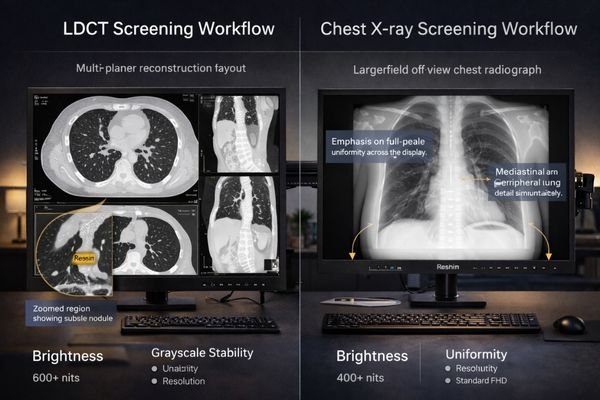
Different modality workflows push the monitor in different ways:
LDCT Screening Requirements
LDCT-based screening benefits from stable grayscale behavior during long sessions, sufficient resolution to support multi-series layouts, and efficient side-by-side comparison of current and prior studies. Because readers scroll through thin-slice data and repeatedly compare subtle changes, calibrated luminance stability5 and predictable grayscale response often matter more to consistency than peak brightness claims. The goal is that subtle findings do not “shift” in appearance as the session progresses or as cases move between workstations.
Chest X-ray Screening Considerations
Chest X-ray screening emphasizes uniformity and consistent grayscale mapping across the entire panel. Since large-field anatomy is assessed holistically, local non-uniformity can distract interpretation or create false impressions of pathology. High throughput also favors displays that maintain stable calibrated behavior without frequent manual adjustment, helping readers stay consistent across many rapid decisions.
Recommended Reshin high-brightness radiology monitors for lung screening
Selecting appropriate high-brightness radiology monitors requires matching display characteristics to the specific reading patterns and technical requirements of different lung-screening modalities.
A practical way to choose monitors for screening deployments is to assign display roles by workstation function: primary diagnostic review (where grayscale consistency and calibration stability are most critical), AI-assisted review (where overlay legibility and color elements may matter more), multi-window review (where workspace density is the priority), and supporting stations (where stable clinical presentation is needed without over-specifying the role).
| Clinical Role / Application | Usage Pattern | Display Requirements | Recommended Model | Key Integration Considerations |
|---|---|---|---|---|
| LDCT Primary Diagnostic | Extended thin-slice review, nodule tracking | Sustained grayscale stability, multi-series layout | MD52G | 21.3" 5MP (2048×2560), 500 cd/m² (panel spec) |
| General Screening Diagnostic | Balanced LDCT/X-ray workflow | Practical grayscale performance, cost efficiency | MD33G | 21.3" 3MP (1536×2048), 500 cd/m² (panel spec) |
| AI-Assisted Screening | Color overlays, heatmaps, triage workflows | Overlay legibility, color presentation aligned with workflow | MD32C | 21.3" 3MP (1536×2048), 500 cd/m² (panel spec) |
| Multi-Modality High-Density | Large canvas for priors, AI panels, multi-series | Expansive workspace, high information density | MD120C | 31" 4200×2800, 450 cd/m² (panel spec) |
| Supporting/Secondary Stations | Worklists, reporting, secondary viewing | Stable clinical presentation, cost-sensitive | MD26C | 24" 1920×1200, 350 cd/m² (panel spec) |
Note: Always verify final specifications and calibration requirements against the latest product datasheets and the target screening platform’s assumptions (e.g., DICOM GSDF behavior, LUT handling, and overlay rendering)
FAQ
1. What is the difference between panel brightness and calibrated luminance?
Panel brightness is a manufacturer specification for maximum luminance capability, while calibrated luminance refers to the controlled, repeatable luminance level used for clinical reading after calibration. Screening programs benefit most when calibrated luminance remains stable over time and across workstations.
2. What does DICOM GSDF mean for lung-screening displays?
DICOM GSDF (Grayscale Standard Display Function) defines a standardized grayscale response curve so that grayscale steps are presented predictably. For LDCT screening, consistent GSDF behavior helps preserve subtle density differences and reduces variability between stations.
3. Why can the same LDCT case look different on different screening platforms?
Platforms may apply different LUT behavior, default window/level presets, and overlay rendering logic. If one workflow assumes monitor-side calibration while another relies more on application-side presentation, subtle grayscale appearance and overlay legibility can change even with the same dataset.
4. Should lung screening use grayscale or color diagnostic monitors?
Grayscale displays are often preferred when the primary task is subtle lesion detection and consistent grayscale perception. Color-capable diagnostic monitors are valuable when AI overlays, color-coded triage, or multi-modality UI elements are central to the workflow.
5. What is the most common deployment issue in multi-site screening programs?
The most common issue is presentation variability—differences in ambient light, calibration practices, and luminance stability across rooms and sites. Standardizing calibration behavior and ensuring stable luminance over time help improve consistency and reader confidence.
Conclusion
Lung-screening systems create distinct requirements for high-brightness radiology monitors based on modality focus, workflow design, and presentation assumptions. LDCT programs emphasize stable calibrated luminance and predictable grayscale behavior to support consistent perception of subtle findings across long sessions, while chest X-ray screening prioritizes full-panel uniformity and consistent grayscale mapping for whole-field assessment. AI-assisted workflows add overlay legibility requirements that further increase the importance of stable luminance behavior and consistent contrast handling.
Reshin’s engineering support focuses on aligning display selection and calibration strategy with the actual screening workflow—helping teams avoid selecting monitors by generic specifications alone and improving consistency across multi-workstation deployments.
✉️ info@reshinmonitors.com
🌐 https://reshinmonitors.com/
-
This resource will provide insights into the importance of grayscale mapping in ensuring accurate medical imaging results. ↩
-
This resource provides insights into the effectiveness of Chest X-ray screening, crucial for understanding its role in public health. ↩
-
Understanding higher luminance can enhance your knowledge of visual clarity in busy radiology settings. ↩
-
Understanding DICOM GSDF is crucial for ensuring accurate grayscale representation in diagnostic systems. ↩
-
Understanding calibrated luminance stability is crucial for ensuring accurate image interpretation in medical diagnostics. ↩



