Fluorescence-guided surgery introduces requirements for display selection and configuration that go beyond standard surgical viewing because success depends on making faint signals reliably visible and keeping presentation consistent through frequent mode transitions.
Fluorescence-guided surgery requires surgical monitors to support stable low-level contrast discrimination, consistent color handling across white-light and fluorescence modes, minimal switching latency, and predictable behavior during the frequent state transitions that occur throughout procedures. These requirements extend beyond basic image quality to include system-level reliability, repeatable modes, and stable overlay presentation.
Fluorescence workflows often expose weaknesses in displays and signal chains that are not obvious in standard surgical visualization. Reliability comes from controlled configuration and validation of the exact chain used in the OR—especially across switching, reboot, and wake events where mode drift and renegotiation tend to appear.
What Makes Fluorescence-Guided Surgery Display Different from Standard White-Light Viewing?
Fluorescence applications add critical information layers that require specialized display considerations.
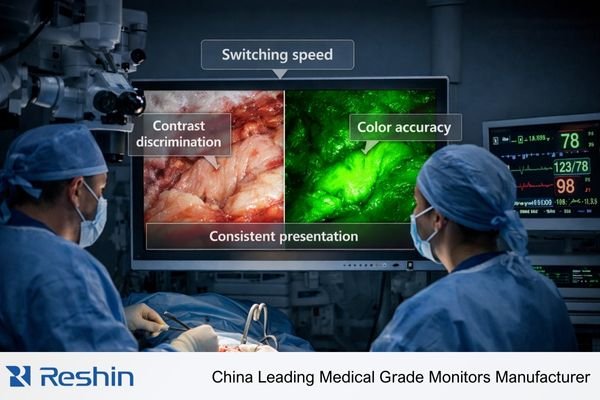
Fluorescence-guided surgery adds a second information-critical image layer with faint signals that must remain visually separable from background tissue while surgeons switch between viewing modes in real time. Monitors must preserve subtle intensity differences, maintain consistent color appearance across modes, and avoid presentation drift during switching events that could undermine decision-making.

In OR video chain configurations, displays that look adequate for white-light viewing can struggle with fluorescence because processing behaviors or mode instability become more significant when subtle cues guide targeting, margin awareness, or navigation decisions.
Multi-Layer Information Processing
Fluorescence-guided surgery1 requires displays that can present multiple information layers without degrading the visibility of either white-light anatomy or fluorescence signals. This places emphasis on controlled processing so image enhancement does not conflict with faint-signal preservation or create misleading visual artifacts.
Real-Time Mode Switching
Teams often switch between white-light and fluorescence views during procedures, which makes fast, predictable transitions essential. Displays should avoid temporary signal loss, slow re-lock behavior, or inconsistent presets that interrupt visual flow during critical moments.
Subtle Signal Preservation
Fluorescence signals are often faint, so the monitor must support strong near-black detail visibility and stable grayscale behavior while avoiding aggressive enhancement that can wash out critical information or introduce false structure.
Which Image Quality Parameters Are Most Critical for Fluorescence Signals?
Specific display characteristics become essential for reliable fluorescence visualization.
Fluorescence visibility depends on stable low-level contrast discrimination, controlled image processing that preserves faint signals, sufficient brightness headroom for readable white-light scenes, and consistent color handling that maintains channel separation in overlay and mixed-mode viewing without unintended hue shifts.

Fluorescence imaging display performance is especially sensitive to how the monitor behaves in low luminance regions and how consistently it renders overlays or pseudo-color mapping. The priority is not “maximum processing,” but stable and repeatable presentation that keeps the fluorescence cue separable from background tissue.
Low-Level Contrast Performance
Fluorescence signals can sit close to the noise floor, so reliable near-black detail visibility and consistent grayscale response are essential. Overly aggressive processing may compress mid-tones or alter local contrast in ways that reduce separability between signal and background.
Brightness Headroom Management
The display should provide sufficient brightness headroom2 so white-light scenes remain readable under typical OR lighting while still leaving dynamic range for fluorescence cues to stand out. The practical goal is stable separation without forcing extreme camera gain or unstable in-system enhancement.
Color Channel Integrity
Overlays, pseudo-color mapping, and mixed-mode views require consistent color handling so channel separation remains reliable and hue does not drift across transitions. Unintended color shifts can make the same fluorescence scene harder to interpret and harder to compare across rooms.
Processing Consistency
Picture presets should be predictable and controlled so that a fluorescence scene appears consistent across mode transitions. Avoiding unexpected changes in processing behavior is as important as the underlying panel characteristics.
How Do Latency, Switching, and Mode Consistency Affect Fluorescence Workflow?
Temporal performance characteristics become critical in fluorescence applications.
Fluorescence-guided surgery is highly sensitive to delay and instability because teams switch modes frequently and rely on immediate visual feedback during instrument movement. Even small latency increases, intermittent signal loss, or slow re-lock behavior can interrupt surgical rhythm, while silent mode changes can make identical scenes appear different across transitions.

Fluorescence workflows raise the operational bar: switching must be fast and repeatable, and the same input path must return to the same timing, encoding, and picture behavior after every transition. When the chain renegotiates into a different mode—or a different preset is applied automatically—clinicians lose confidence because the same scene can look different without any obvious warning.
Switching Latency Impact
Fast mode transitions matter because delays during switching can interrupt visual flow when instruments are positioned relative to fluorescence-guided targets. Practical performance expectations should be defined in the context of the room’s workflow, then validated on the actual chain used during cases.
Mode Stability Requirements
Instability that triggers silent changes in timing, encoding, range handling, or picture presets can alter perceived contrast and overlay behavior. For fluorescence, “same mode every time” is the objective so scenes remain comparable across switching events.
Renegotiation Minimization
Reduce unnecessary renegotiation by keeping routing paths consistent, minimizing adapters where possible, and validating intermediate devices (switchers/extenders/KVMs) as part of the baseline. The goal is fast, repeatable locking to the same known-good mode.
Real-Time Feedback Preservation3
Because fluorescence guidance depends on immediate visual feedback, avoid workflows where the chain regularly re-locks, drops frames, or changes presentation characteristics during routine transitions. Stable behavior across boot, wake, and switching is a primary acceptance criterion.
What Validation and QA Steps Should You Add for Fluorescence-Ready Displays?
Fluorescence applications require systematic validation beyond standard display testing.
Fluorescence readiness should be treated as system-level acceptance: define the workflow, lock the intended mode, validate behavior across cold boot/wake/switching/routing transitions, verify overlay and preset consistency, document the baseline for the exact surgical signal path, and re-verify after change.
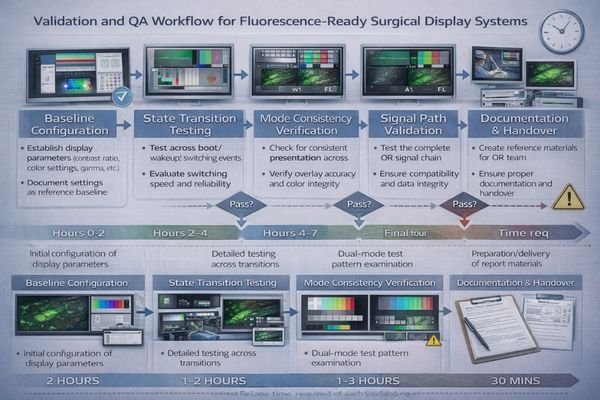
Fluorescence performance should be evaluated under the conditions that occur during real procedures, not only in ideal lab setups. The weakest link is often the signal chain rather than the panel, so validation should focus on repeatability across the transitions that commonly trigger mode drift.
State Transition Testing
Test across cold boot, wake events, input switching, and routing changes to confirm the same source selects the same mode and the monitor re-locks consistently. Repeatability across these transitions is a stronger indicator of clinical readiness than a single successful connection.
Processing Preset Verification
Confirm that picture presets remain stable and that any clinical overlay or pseudo-color presentation behaves consistently across switching and reconnection events. The objective is preventing silent processing changes that make the same fluorescence scene appear different.
Baseline Documentation
Document baseline settings4 for the exact input path and any intermediate devices used in the OR, including port/path definitions and the intended timing/encoding/preset. This documentation becomes the reference for troubleshooting and for restoring known-good behavior after maintenance.
Ongoing Maintenance Protocols
Re-verify after firmware updates, source replacements, switcher/extender changes, or routing reconfiguration to prevent configuration drift that could quietly degrade fluorescence visibility or switching reliability over time.
What Surgical Monitors Are Better Suited for Fluorescence-Guided Surgery Setups?
Display selection should prioritize the specific requirements of fluorescence applications and OR workflows.
Selection should start from the dominant fluorescence workflow patterns and real OR signal chain requirements rather than maximum specification comparisons.
| Clinical Role / Application | Usage Pattern | Display Requirements | Recommended Model | Key Integration Considerations |
|---|---|---|---|---|
| Primary Fluorescence Display | Frequent mode switching, real-time feedback | Fast switching, stable processing, excellent contrast | MS430PC | Minimal latency, consistent mode handling |
| Large Format Team Display | Multi-person viewing, collaborative procedures | Large screen, stable fluorescence visibility | MS550P | Team visibility, consistent processing across viewing angles |
| Multi-Input Surgical Display | Multiple sources, complex routing | Reliable input switching, stable renegotiation | MS321PB | Robust switching, predictable mode retention |
| Compact Fluorescence Monitor | Space-constrained applications | Reliable performance, consistent behavior | MS321PC | Stable operation, predictable processing |
| High-Resolution Fluorescence Display | Detailed visualization, precision applications | High resolution, excellent contrast discrimination | MS275PA | Fine detail resolution, stable low-level contrast |
Consider the dominant fluorescence workflow requirements including switching frequency, multiple source integration, and routing complexity that drive fast switching, stable renegotiation, and consistent processing needs. Evaluate viewing distance and team visibility requirements that affect screen size selection while maintaining fluorescence signal readability.
Plan interface strategies that maintain healthy bandwidth margins, minimize adapters that can affect negotiation, and reduce renegotiation triggers when switchers or extenders are necessary for OR integration requirements.
Prioritize displays that support repeatable configuration with lockable picture modes, stable behavior across power cycles, cleaning protocols compatible with OR requirements, and serviceability approaches that enable quick restoration of verified baselines when units require replacement.
FAQ
Is higher brightness always better for fluorescence-guided surgery?
Not by itself—brightness helps maintain headroom in white-light scenes, but fluorescence visibility also depends on stable low-level contrast, consistent processing, and repeatable modes across switching.
Why does the fluorescence view sometimes look different after switching inputs?
Input switching can trigger renegotiation and silent mode changes (timing/encoding/range or picture presets), which can alter overlays or perceived contrast even if an image still appears.
Do KVMs, extenders, or switchers increase fluorescence-related risk?
They can, because they may change capability exposure and negotiation timing, which affects mode selection and switching stability; validate the exact chain used in surgery.
What is the most important acceptance test for fluorescence-ready monitors?
Repeatability across state transitions—confirm the same source selects the same mode and the monitor re-locks consistently after boot, wake, and switching, with stable overlay appearance.
Can auto "enhancement" features harm fluorescence interpretation?
Yes—aggressive processing can compress mid-tones or alter channel separation; prioritize controlled, consistent presets and avoid unexpected processing changes during surgery.
Should fluorescence setups be re-verified after updates or replacements?
Yes—firmware updates, source replacements, or routing changes can reintroduce mode drift; re-verify the same baseline and transition behavior to keep performance predictable.
Conclusion
Fluorescence-guided surgery elevates surgical monitor requirements by making subtle signal visibility, fast switching performance, and repeatable behavior essential to reliable OR workflows. The most important capabilities are stable low-level contrast discrimination, consistent color handling, minimal added latency, and mode consistency across the frequent transitions that occur during cases.
At Reshin, we approach fluorescence readiness as a system requirement: define the workflow, lock the intended mode, validate transitions on the exact OR signal chain, document the baseline, and re-verify after change. By combining controlled configuration with repeatable acceptance testing and maintenance checks, surgical teams can reduce interruptions and maintain confidence that fluorescence presentation remains consistent throughout procedures.
✉️ info@reshinmonitors.com
🌐 https://reshinmonitors.com/
-
Explore this link to understand how to optimize displays for fluorescence-guided surgery, ensuring better outcomes. ↩
-
Understanding brightness headroom is crucial for ensuring optimal visibility in various lighting conditions. ↩
-
Exploring real-time feedback preservation can help you maintain visual clarity and stability during important transitions. ↩
-
Documenting baseline settings is essential for troubleshooting and maintaining optimal performance in medical equipment. ↩