Accurate grayscale is essential, but what about color? A subtle drift in color on a medical display can misrepresent tissue health, quietly leading to flawed clinical judgments and diagnostic errors.
Color shift quietly bends clinical judgment. DICOM guards grayscale, not color, so manage the whole chain: stable white point, BT.709/BT.2020, AR-bonded optics, ambient-light control, luminance stabilization, and clean 12G-SDI/HDMI 4:4:4. Lock profiles and check multi-view consistency. With routine QA, screens stay honest—and decisions stay precise.
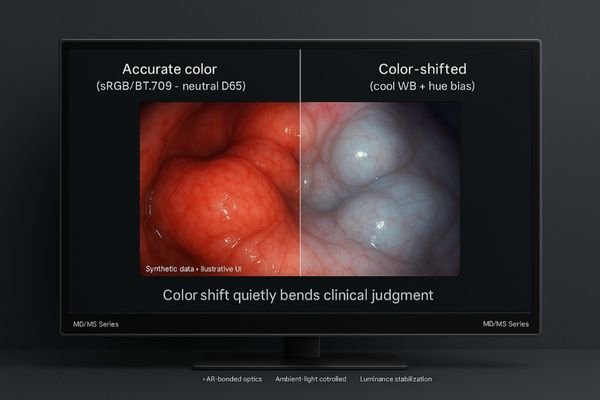
We often focus on DICOM Part 14 to ensure grayscale accuracy, but this standard does not govern color fidelity1. In specialties like endoscopy, pathology, and surgery, color is not merely cosmetic—it is critical clinical data. A monitor that shows a slight color shift can mask the difference between healthy and ischemic tissue, or obscure subtle bleeding. To ensure patient safety and diagnostic confidence, we must manage the entire color pipeline2, from the video source to the surgeon’s or radiologist’s eye. This requires a deeper look into the technologies and workflows that preserve color integrity.
Endoscopy & Surgery: How Color Shift Distorts Tissue Cues
In the operating room, surgeons rely on color to judge tissue health. A monitor with inaccurate color can flatten contrast and hide critical cues, delaying decisions and increasing procedural risk.
Color shift threatens surgical accuracy by distorting the visual cues surgeons use to assess tissue planes, perfusion, and subtle bleeding. Managing the entire color pipeline from camera to screen is essential for clinical confidence.

During an endoscopic procedure, a surgeon’s decisions are guided by visual information where hue and saturation are paramount. A subtle tinge of yellow may indicate bile, while a shift toward blue could signal ischemia. If the surgical monitor’s color drifts, these vital cues can be lost. Healthy pink mucosa might appear washed out, or the boundaries of a lesion could become indistinct. This compromises the surgeon’s ability to act with precision and confidence. To mitigate this risk, modern surgical displays must be engineered for color fidelity. A monitor like the MS321PB achieves this with a combination of technologies. It supports wide color gamuts3 like BT.2020, uses AR glass and optical bonding to defeat glare, and maintains signal integrity through professional 12G-SDI inputs. By ensuring the color pipeline is consistent and accurate, we reduce the chance of misinterpretation and support safer surgical outcomes.
Beyond DICOM: Managing Color Accuracy, Not Just Grayscale
Many assume that a DICOM-compliant monitor guarantees all-around visual accuracy. This is a dangerous oversimplification, as DICOM Part 14 only standardizes the perception of grayscale values.
Because DICOM only governs grayscale, color-critical workflows require separate color management. This means using displays that support calibrated color gamuts like BT.709, ensuring consistent performance across different modalities.
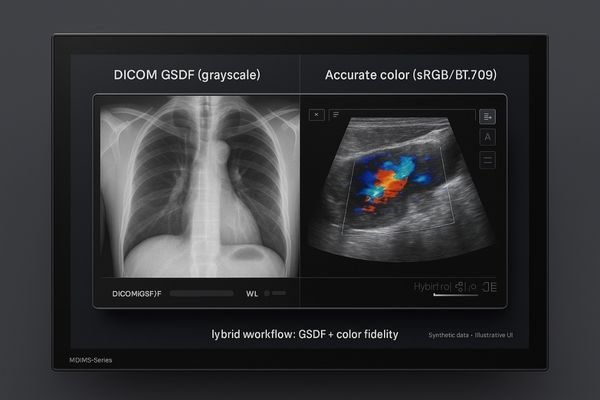
While DICOM compliance4 is non-negotiable for primary diagnosis in radiology, it does not address the challenges of color reproduction5. This creates a gap in quality assurance for disciplines that rely on color information, such as pathology, dermatology, and multi-modality radiology. For example, when a PACS workstation is used to review both a grayscale CT scan and a color Doppler ultrasound, the display must perform two distinct tasks accurately. It needs to render the CT according to the DICOM GSDF curve while also displaying the ultrasound’s color flow data according to a standard like sRGB or BT.709. A specialized display like the MD46C is designed for this hybrid workflow. It provides both hardware-based DICOM calibration for grayscale images and separate, accurate color gamma modes. This dual capability prevents hue bias that could mislead clinical judgment and ensures that readings are consistent, whether an image is viewed in the main reading room or a multi-disciplinary team meeting.
Ambient Light, AR Glass, and Optical Bonding in Color Perception
A perfectly calibrated monitor can still display inaccurate color in a poorly controlled environment. Reflections from room lighting create veiling glare, which desaturates colors and compresses contrast.
Perceived color is shaped by the viewing environment. A combination of AR glass, optical bonding, and ambient light compensation is essential to maintain color fidelity and contrast in real-world clinical settings.
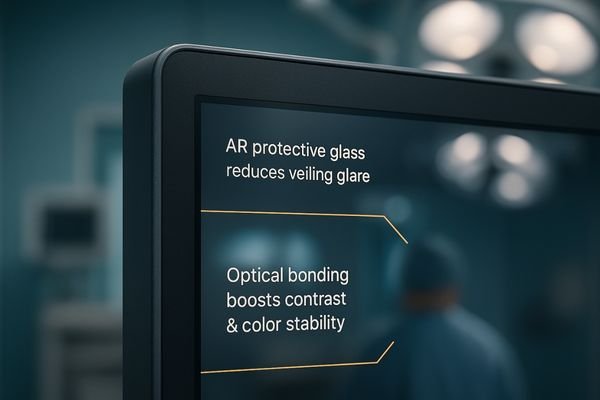
The color a clinician perceives is a product of both the monitor’s output and the ambient conditions of the room. Bright overhead lights, windows, and even reflections from clothing can alter the way colors appear on screen. High-performance medical displays combat this with a system of optical technologies. The first line of defense is anti-reflection (AR) coated glass6, which minimizes surface glare. The next step is optical bonding, which eliminates the internal air gap between the glass and the LCD panel. This prevents internal reflections and significantly improves contrast, making colors appear richer and blacks deeper, especially when viewed from an angle. Finally, an ambient light sensor7 can allow the monitor to intelligently adjust its luminance to maintain a consistent white point as room lighting changes. An OR-grade monitor like the MS321PC integrates these features into a sealed, flat-front design. This robust optical system ensures that what the clinician sees on the screen remains true, regardless of the challenging lighting conditions of the operating room.
Stability Over Time: Aging, Luminance Drift, and Auto-QA
A medical display’s color and brightness are not static. Over thousands of hours of use, the backlight ages, panel characteristics change, and performance can drift away from its initial calibrated state.
Color accuracy degrades silently over time due to aging and thermal stress. Monitors with built-in luminance stabilization and automated quality assurance systems are crucial for maintaining diagnostic consistency throughout the display’s lifecycle.
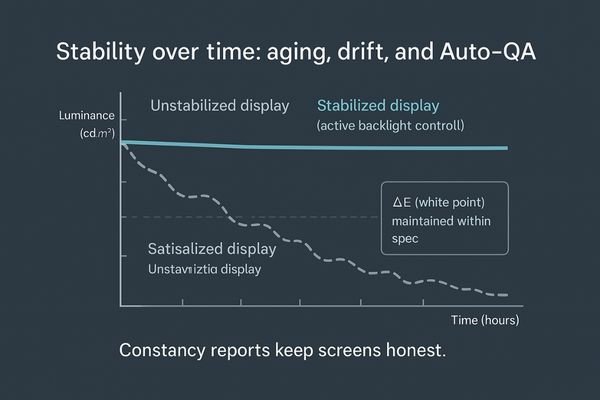
Maintaining color and grayscale accuracy8 is a continuous process, not a one-time setup. As a monitor ages, its peak luminance can decrease and its white point can shift, causing colors to appear differently. This drift is often too gradual for the human eye to notice day-to-day, but it can accumulate into a significant source of diagnostic inconsistency over time. To counteract this, high-quality medical displays incorporate active stabilization technologies. Internal sensors continuously monitor the backlight’s output and make real-time adjustments to maintain constant luminance. For diagnostic monitors like the MD33G, this is often paired with a front sensor that can run automated quality assurance (QA) checks9 according to a schedule. This Auto-QA system verifies that the display remains compliant with a standard like DICOM and logs the results for auditing purposes. This approach reduces the total cost of ownership by minimizing manual intervention and protects clinical accuracy by ensuring the display performs predictably for years.
Multi-View Workflows: Keep PIP/PBP Colors Consistent
Picture-in-Picture (PIP) and Picture-by-Picture (PBP) modes are now standard in ORs. However, if each window on the screen uses a different color profile, it can lead to confusing and misleading comparisons.
When using multi-view layouts, each window must maintain consistent color and gamma profiles. This ensures that visual cues from different sources can be compared reliably, reducing cognitive load during critical procedures.
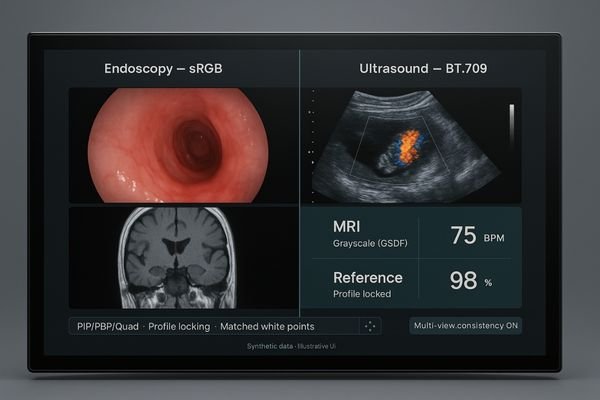
In today’s integrated operating rooms, surgeons frequently need to view multiple sources at once—for example, a live endoscopic feed, a preoperative MRI, vital signs, and an ultrasound image. While multi-view functionality10 is common, ensuring visual consistency across all windows is a more complex challenge. If the monitor applies different color temperatures or gamma curves to each input, a surgeon might misinterpret tissue perfusion or bleeding when comparing the live feed to a reference image. A top-tier surgical display11 like the MS550P is designed to solve this problem. It allows administrators to lock color profiles for each input and ensures that these profiles are maintained consistently across different multi-view layouts, whether in PIP, PBP, or quad-view mode. This capability ensures that all visual information is presented on a level playing field, allowing for direct and reliable comparisons without introducing cognitive friction or the risk of misinterpretation.
| Multi-View Feature | Clinical Importance |
|---|---|
| Consistent Color Profiles | Ensures that tissue in the live view can be reliably compared to reference images. |
| Profile Locking | Prevents accidental changes to color settings during a procedure. |
| Flexible Layouts (PIP/PBP/Quad) | Allows for customizable display of all necessary information on a single screen. |
| Clear Source Labeling | Reduces confusion by clearly identifying which video feed is in which window. |
Signal Integrity Matters: 12G-SDI vs HDMI and Chroma Sampling
The way video data is compressed and transmitted can impact the final color on screen. Using a consumer-grade signal path can inadvertently strip out subtle color information before it ever reaches the display.
A clean signal path is the first step to accurate color. Professional interfaces like 12G-SDI and properly implemented HDMI 2.0 preserve full color information, preventing the subtle hue loss that can mask clinical details.

A monitor can only display the information it receives. If the video signal has been compromised during transmission, even a perfectly calibrated display will show inaccurate color. The choice of interface and cable is critical. For demanding 4K surgical video, 12G-SDI is the professional standard. It provides a robust, locking connection capable of carrying an uncompressed 4K signal over long distances, which is essential for maintaining signal integrity in an environment with high electromagnetic interference. While HDMI 2.0 is also capable of carrying a 4K signal, its performance is highly dependent on cable quality and length. A more subtle issue is chroma subsampling1. Many systems use 4:2:2 or 4:2:0 subsampling to reduce bandwidth, which discards some color information. For maximum fidelity, a 4:4:4 signal path, where full color information is preserved, is ideal. A monitor like the MS322PB supports both 12G-SDI2 and full-bandwidth HDMI 2.0 inputs, ensuring that the cleanest possible signal is received. This prevents the loss of subtle hues that might indicate ischemia or thermal injury.
Conclusion
Managing color shift requires a holistic approach that goes beyond grayscale calibration to include color management, robust optics, automated QA, and a clean, reliable signal path. 🌈
👉 For advanced color-stable medical display solutions, contact martin@reshinmonitors.com.
MS321PB
-
Understanding color fidelity is crucial for accurate diagnostics in medical imaging, ensuring patient safety and effective treatment. ↩ ↩
-
Exploring the management of the color pipeline can enhance your knowledge of preserving color integrity in critical medical procedures. ↩ ↩
-
Exploring wide color gamuts reveals how they improve color accuracy, which is vital for precise surgical decisions. ↩
-
Understanding DICOM compliance is crucial for ensuring accurate medical imaging and diagnosis. ↩
-
Exploring color reproduction in medical imaging can enhance diagnostic accuracy and improve patient outcomes. ↩
-
Understanding AR coated glass can enhance your knowledge of display technology and its impact on color accuracy. ↩
-
Exploring ambient light sensors will reveal how they optimize display performance in varying lighting conditions. ↩
-
Explore this link to learn effective techniques for ensuring consistent color and grayscale accuracy in your displays. ↩
-
Discover how automated QA checks enhance monitor reliability and compliance, ensuring optimal performance over time. ↩
-
Understanding multi-view functionality can enhance your knowledge of surgical displays and their importance in operating rooms. ↩
-
Exploring the benefits of surgical displays can provide insights into their critical role in improving surgical outcomes and patient safety. ↩



