During ENT or urology surgery, a standard monitor can create visual ambiguity. Uncontrolled reflections and inaccurate colors obscure critical tissue details, increasing procedural risk and slowing down the operation.
A top endoscopy monitor for ENT and urology ensures safe, efficient surgery and successful OEM integration. This requires mastering optical clarity, true color rendition, low-latency video, and OR-grade reliability—the core criteria for clinical excellence.
Recommended models

Selecting the right display for endoscopic surgery is about ensuring predictable visibility, not just chasing high resolution. The monitor is a critical instrument that directly impacts a surgeon’s ability to identify anatomy, control bleeding, and perform delicate dissections with confidence. An effective ENT surgery display1 or urology endoscopy monitor2 must deliver a stable, clear, and accurate image under the demanding conditions of the operating room. Focusing on the core technical criteria that translate directly into clinical safety and efficiency is paramount.
Key Criteria Defining a Safe ENT Surgery Display
An unpredictable display creates constant visual uncertainty. Surgeons and staff waste mental energy compensating for shifting brightness or poor contrast, which increases the risk of error and slows down room turnover.
A safe ENT surgery display is defined by predictable visibility. This includes stable luminance, controlled reflections, consistent gamma, a robust physical design, and automated constancy checks to reduce errors and improve OR efficiency.
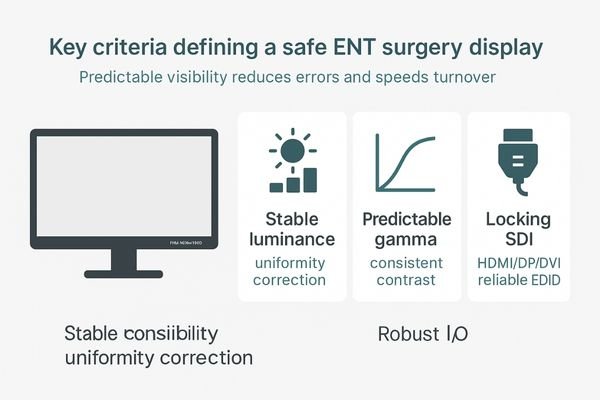
The foundation of a safe endoscopy monitor is its ability to provide a consistently reliable image. This begins with stable luminance3 across the entire panel, ensuring that no part of the screen is dimmer or brighter than another. It requires controlled reflections and a consistent gamma curve so that tissue boundaries and instrument edges do not appear to shift as viewing angles change. The physical design is equally important. In space-constrained OR carts, a compact housing4 and secure mounting are essential. Robust connectors and standardized EDID behavior reduce the chance of signal loss or handshake failures when turning a room around. For OEM deployments, a monitor like the MS192S provides this baseline reliability in a smaller footprint. Ultimately, when these fundamentals are met, the surgical team can stop compensating for the screen and focus entirely on the patient, reducing cognitive load and the risk of error.
Optical Clarity: AR Glass, Bonding, and Anti-Liquid Design
Glare and internal reflections from a standard monitor can obscure fine details. This veiling glare can be particularly problematic when viewing wet, glossy mucosal surfaces, forcing surgeons to guess at critical anatomy.
True optical clarity is a system property. It combines anti-reflection (AR) glass and optical bonding to deepen blacks and improve off-axis contrast, while a flat-front, anti-liquid design ensures hygiene and durability.
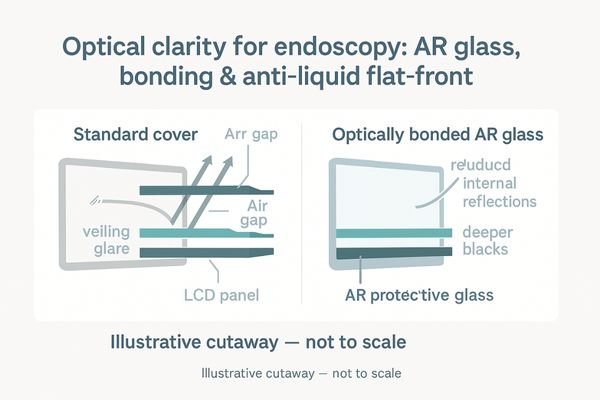
The optical performance of an endoscopy monitor is determined by how its components work together as a system. The first layer is anti-reflection (AR) protective glass5, which is engineered to minimize veiling glare from overhead surgical lights while preserving the micro-contrast needed to visualize fine textures on mucosal surfaces. The second critical element is optical bonding6. This process eliminates the air gap between the glass and the LCD panel, which prevents internal reflections, deepens perceived black levels, and dramatically improves contrast when the screen is viewed from an off-axis angle by multiple staff members. This combination of AR glass and bonding ensures that fine capillaries and small bleeders remain crisp and distinct. Finally, a true flat-front design without a raised bezel is essential for hygiene, as it allows for fast, effective wipe-downs between cases and prevents liquid ingress. These optical features directly translate to quicker identification of bleeding points and safer, more confident dissection.
True Color for Mucosa and Bleeding Assessment in Surgery
Inaccurate color is not just a cosmetic issue; it is a clinical risk. An oversaturated or poorly calibrated display can mask the subtle hue changes that indicate ischemia, inflammation, or bile staining, leading to flawed judgments.
Clinical decisions in ENT and urology rely on accurate color. A credible endoscopy monitor must render sRGB/BT.709 faithfully, maintain neutral whites, and provide screen-wide uniformity to ensure correct tissue assessment.
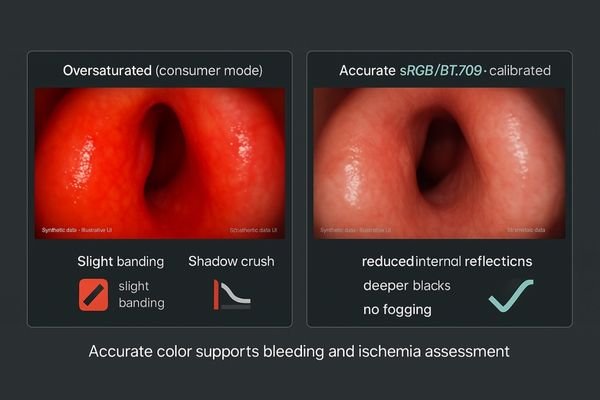
In many surgical specialties, color is clinical data. This is especially true in ENT and urology, where surgeons depend on subtle shifts in tissue hue to guide their actions. A trustworthy endoscopy monitor7 must be factory-calibrated to render color spaces like sRGB and BT.709 with high fidelity. This means maintaining neutral white points and avoiding the oversaturation that can artificially enhance reds but obscure important surface textures. Advanced monitors also employ uniformity correction to ensure that tissue appears the same color whether it is at the center or the corner of the screen, removing location-dependent bias from a surgeon’s assessment. This can be enhanced with a model such as the MS220S. When paired with a consistent gamma curve, this color accuracy8 ensures that instruments and tissue planes retain their intended contrast. In teaching environments, this faithful color reproduction improves confidence transfer, as trainees can trust that the visual landmarks they see are identical to what their trainer is describing.
Low-Latency Processing and Motion Handling at 1080p60 for Endoscopy Video
Any perceptible delay between a surgeon’s hand movement and the on-screen image is disorienting. This lag, known as latency, disrupts hand-eye coordination and can compromise the precision of delicate surgical tasks.
Low-latency video processing at a 1080p60 signal rate is mandatory for endoscope-driven surgery. Minimal delay and clean motion handling ensure that hand-eye coordination remains synchronized, which is critical for procedural safety.
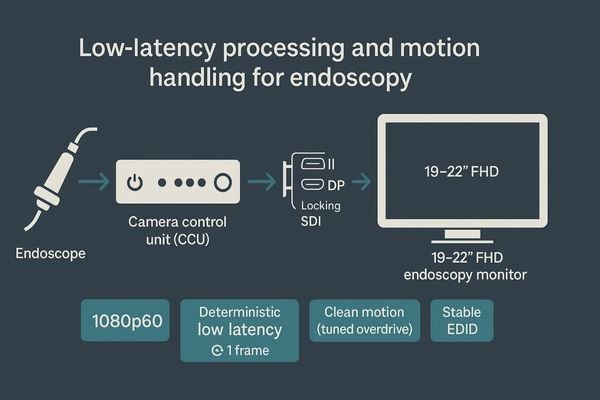
In minimally invasive surgery, timing is everything. The visual feedback loop from the endoscope to the surgeon’s eyes must be as close to instantaneous as possible. An effective endoscopy monitor9 must be engineered with minimal internal processing buffers to ensure low end-to-end latency10. This keeps the surgeon’s hands perfectly synchronized with the on-screen image, which is vital for precise maneuvers like suction, clipping, and cautery, especially within the narrow anatomical confines of ENT and urology procedures. Beyond latency, the monitor must also handle motion cleanly. This involves careful tuning of the panel’s overdrive circuit to minimize motion blur during fast camera pans without creating "overshoot" artifacts like bright halos around instruments. Predictable video timing, supported by stable clocking and reliable EDID handshakes, translates directly into safer and more confident surgical action where millimeters matter.
| Feature | Clinical Benefit in Endoscopy |
|---|---|
| Low End-to-End Latency | Maintains seamless hand-eye coordination for precise instrument control. |
| Optimized Motion Handling | Prevents motion blur during camera pans and avoids visual artifacts around tools. |
| Stable Signal Sync (1080p60) | Reduces black screens and sync issues during scope swaps or source changes. |
Flexible Multi-Input, Multi-View for Endoscope-Driven OR Workflows and Teaching
Modern operating rooms are complex multimedia environments. A single-input monitor creates workflow bottlenecks, forcing staff to swap cables and use fragile dongles to view different sources.
Workflow efficiency demands flexible multi-input connectivity and multi-view capabilities. This allows for the simultaneous display of a live scope feed alongside ultrasound, vitals, or reference images, streamlining both surgery and teaching.

A surgical display should be a hub, not a bottleneck. To achieve this, it must offer a comprehensive range of inputs, including professional-grade SDI, common digital standards like DVI and HDMI, and even legacy analog ports to ensure compatibility with any piece of equipment in the OR. This versatility eliminates the need for failure-prone adapters and simplifies setup. Beyond inputs, powerful multi-view functions11 like Picture-in-Picture (PIP)12 and Picture-by-Picture (PBP) are crucial for modern workflows. These features allow a surgeon to view the live endoscopic feed while simultaneously referencing a CT scan, an ultrasound image, or patient vital signs on the same screen. For teaching, this makes it possible to show a trainee a reference video alongside the live procedure. When this flexibility is combined with workflow-centric presets that recall specific layouts and settings with a single touch, the display becomes a quiet enabler of a safer, more efficient surgical environment.
Integration, EMC, and OR-Grade Reliability Over Time for OEM Deployments
For medical device manufacturers (OEMs), a monitor is a component of a larger system. Its long-term reliability, regulatory compliance, and serviceability are just as important as its optical performance.
Successful OEM deployments depend on a display platform engineered for integration. This includes proven electromagnetic compatibility (EMC), robust thermal management, long-term panel continuity, and features that support remote fleet management.
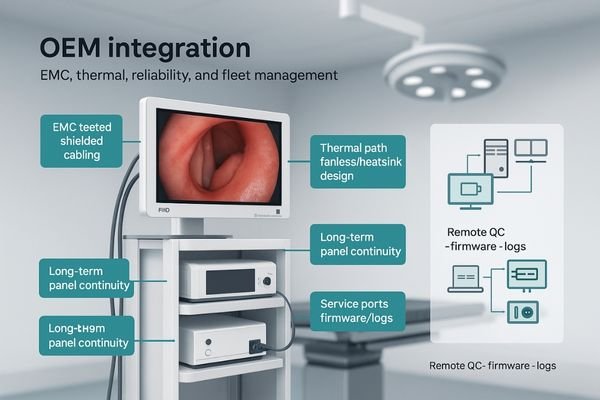
When an endoscopy monitor is integrated into a surgical tower or system, it becomes part of a certified medical device. Therefore, it must be engineered as a reliable platform, not a one-off product. This starts with proven electromagnetic compatibility (EMC)13, ensuring the display does not interfere with other critical OR equipment. It requires robust thermal management14 to maintain stability even within sealed enclosures. For OEMs building a product line, supply chain stability is paramount; a commitment to long-term panel continuity prevents the need for costly redesigns and re-validations every few years. Furthermore, the monitor family should support remote fleet management, allowing for centralized logging, firmware updates, and quality control. When a display is designed with clear documentation, serviceable components, and a focus on OR-grade reliability, it allows device makers to focus on their core innovations in scopes and processors, confident that the visualization platform will remain stable and predictable for years to come.
Conclusion
The best ENT and urology endoscopy monitor delivers predictable visibility through AR-bonded optics, true color, low latency, and a design that prioritizes both OR workflow and long-term reliability. 🔍
👉 For customized ENT and urology display solutions, contact martin@reshinmonitors.com.
-
Explore this link to discover top-rated ENT surgery displays that enhance visibility and surgical precision. ↩
-
Learn about essential features of urology endoscopy monitors to ensure safety and efficiency in surgical procedures. ↩
-
Understanding stable luminance is crucial for ensuring high-quality imaging in medical procedures. ↩
-
Exploring the significance of compact housing can enhance your knowledge of space optimization in surgical environments. ↩
-
Explore this link to understand how AR glass enhances visibility and reduces glare in surgical settings. ↩
-
Learn about optical bonding’s role in enhancing contrast and clarity, crucial for effective surgical procedures. ↩
-
Explore this link to discover top-rated endoscopy monitors that ensure accurate color representation, crucial for surgical precision. ↩
-
Understanding color accuracy in surgical monitors can enhance surgical outcomes and training effectiveness, making this resource invaluable. ↩
-
Explore this link to understand the essential features of endoscopy monitors that enhance surgical precision and safety. ↩
-
Discover why low end-to-end latency is crucial for surgical success and how it impacts the surgeon’s performance. ↩
-
Learn about the advantages of multi-view functions in surgical displays, which streamline operations and enhance the surgical experience. ↩
-
Explore how PIP enhances surgical workflows by allowing simultaneous viewing of critical information, improving efficiency and safety. ↩
-
Understanding EMC is crucial for ensuring that medical devices operate safely without interference, making this resource invaluable for device manufacturers. ↩
-
Exploring thermal management can help manufacturers enhance device reliability and performance, ensuring optimal operation in critical environments. ↩



