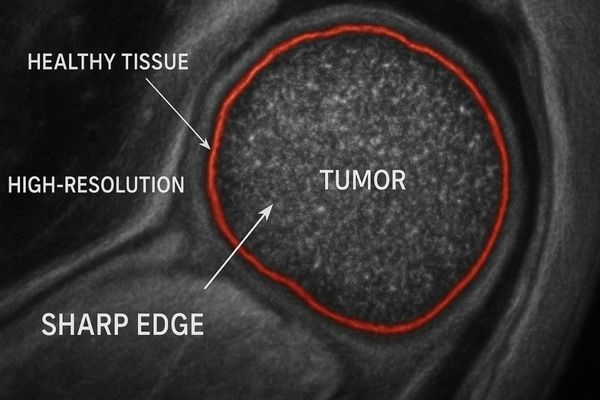
Defining the precise edge of a tumor is a constant challenge. An unclear boundary on a medical image can lead to incomplete resections, directly impacting patient prognosis.
High-resolution medical displays, particularly those with 5 megapixels (MP) or more, are essential for enhancing tumor boundary visualization. They render the subtle texture and density variations between malignant and healthy tissue with superior clarity, which is critical for accurate diagnosis and surgical planning.
The ability to see clearly is the foundation of modern medicine. In oncology, this clarity is not just about seeing an image; it is about interpreting the subtle story told by every pixel. The line between a successful diagnosis and a missed opportunity, or between a complete tumor removal and a recurrence, can be as fine as a few pixels on a screen. That is why the resolution of a medical display1 is not a technical specification to be glossed over. It is a fundamental component of clinical care. In this article, we will examine how display resolution2 directly impacts the ability to identify tumor margins, assess diagnostic images, and plan life-saving surgical procedures.
Why is high resolution critical for accurately identifying tumor margins in medical imaging?
Faint tumor margins can easily blend with surrounding healthy tissue. Missing these subtle visual cues can lead to an inaccurate diagnosis or an incomplete surgical plan, with serious consequences.
High resolution is critical because tumor margins are defined by very subtle gradients in tissue density, texture, and vascularity. A display with a high pixel count can render these minute variations clearly, transforming an ambiguous smudge into a definable and clinically actionable boundary.
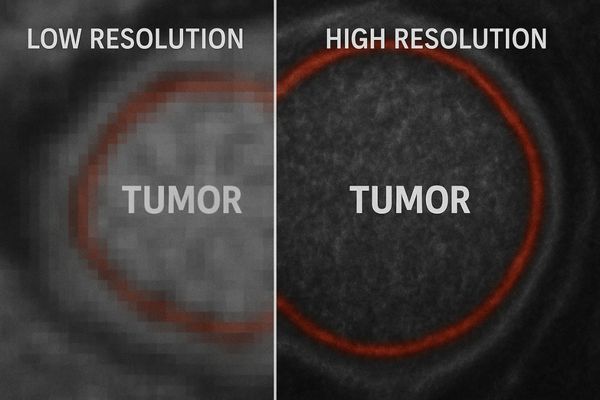
Tumors rarely have perfectly smooth, defined borders. More often, their edges are irregular, with tiny, finger-like projections (spiculations) or areas of subtle infiltration into adjacent tissue. These features are often the key indicators of malignancy and invasiveness. On a low-resolution display, these critical details are lost. The pixels are too large to capture the fine lines and faint changes in grayscale that characterize the tumor’s true extent. The result is an effect called "pixelation" or "blurring," which can make a malignant lesion appear benign or obscure its full size. This forces the clinician to make a judgment based on incomplete information. A high-resolution monitor3 provides the necessary detail to overcome this. It allows for a one-to-one mapping of the image data from the scanner, ensuring that every piece of information captured is visible. For tasks like mammography, where identifying micro-calcifications4 is essential, a display like our MD52G – 5MP Grayscale Mammography Monitor is indispensable. Its high pixel density makes these tiny, crucial indicators stand out.
What minimum pixel count is recommended for detecting subtle differences at tumor edges?
You need to select a new monitor for your oncology department. The technical specifications can be confusing, and making the wrong choice could compromise diagnostic accuracy for your team.
For detecting subtle differences at tumor edges, especially in detailed applications like mammography, a minimum resolution of 5 megapixels (5MP) is the widely accepted recommendation. For reviewing complex, multi-modality studies, 8MP to 12MP displays are increasingly becoming the standard.
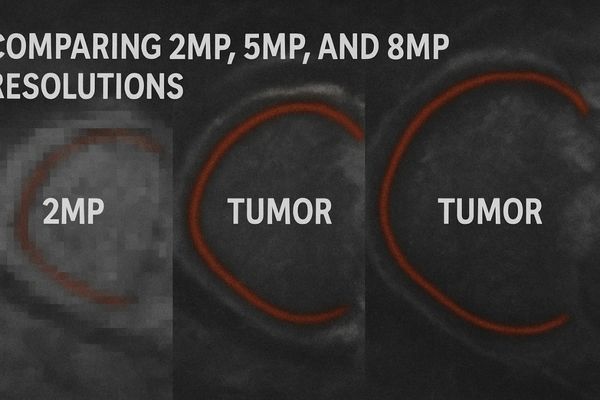
The recommended pixel count for a medical display is directly tied to the clinical application. Different imaging tasks have different requirements for detail. While a 2MP or 3MP monitor may be sufficient for general clinical review, it falls short for primary diagnosis in specialties that rely on detecting minute abnormalities. In mammography, for example, the goal is to spot micro-calcifications that can be smaller than a millimeter. A 5MP display5 provides the pixel density needed to resolve these objects clearly. For radiologists reviewing complex oncology cases that involve fusing images from PET and CT scanners, even more data is present. An MD85CA allows them to view these large, fused datasets on a single screen without losing detail or needing to constantly pan and zoom. This improves workflow efficiency and reduces the risk of missing something important. The choice of resolution is about matching the tool to the task to ensure the highest level of diagnostic confidence is always maintained.
Recommended Resolutions for Oncologic Imaging Tasks
| Resolution | Megapixels (MP) | Primary Application in Oncology |
|---|---|---|
| 2048 x 1536 | 3 MP | General Radiology (CT, MRI), Clinical Review |
| 2560 x 2048 | 5 MP | Mammography, Digital Breast Tomosynthesis, Pathology |
| 3840 x 2160 | 8 MP (4K) | Multi-modality fusion (PET/CT), 3D Reconstruction, Surgical Planning |
| 4200 x 2800 | 12 MP | Advanced Mammography, Tomosynthesis, Large-Format Diagnostics |
How does resolution impact the effectiveness of diagnostic tools like MRI or CT for tumor assessment?
Your hospital invested heavily in a state-of-the-art MRI or CT scanner. However, if the images are viewed on a standard office monitor, you are losing valuable diagnostic information.
A medical display’s resolution is the final, critical link in the imaging chain. If the display has a lower resolution than the imaging modality, crucial data is discarded through down-sampling. A high-resolution monitor ensures that every detail the scanner captures is faithfully presented to the clinician.
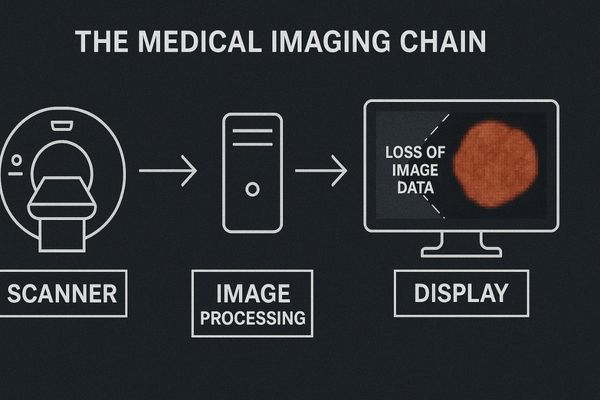
The journey of a medical image from patient to physician is known as the "imaging chain6." It starts with data acquisition at the scanner (CT, MRI), followed by image processing, and ends with interpretation on a display. This chain is only as strong as its weakest link. A hospital can have the most advanced scanner in the world, but if the image is viewed on a low-resolution display, the investment is wasted. Modern scanners generate massive datasets. A single CT slice can contain millions of data points. A display without enough pixels cannot show all this information at once. It is forced to average or discard data, a process known as down-sampling. This effectively blurs the image and erases the fine details that are often most important for tumor assessment. It is like trying to read a detailed map on a tiny, blurry screen. You lose all the nuance. To prevent this loss of information, the display resolution must be sufficient to handle the scanner’s output. A monitor like our MD32C – 3MP Diagnostic Monitor provides a solid foundation for reviewing CT and MRI studies, ensuring the image integrity is maintained from the scanner to the radiologist’s eyes.
Are specialized high-resolution displays, like those from Reshin, necessary for tumor visualization tasks?
You see consumer-grade 4K monitors available at a much lower price. You wonder if they are a viable alternative, but they lack the specific features needed for clinical diagnosis.
Yes, specialized high-resolution medical displays are absolutely necessary. Unlike consumer monitors, they are engineered for clinical accuracy with features like factory DICOM calibration, brightness uniformity, and backlight stabilization, which are essential for visualizing subtle tumor characteristics.
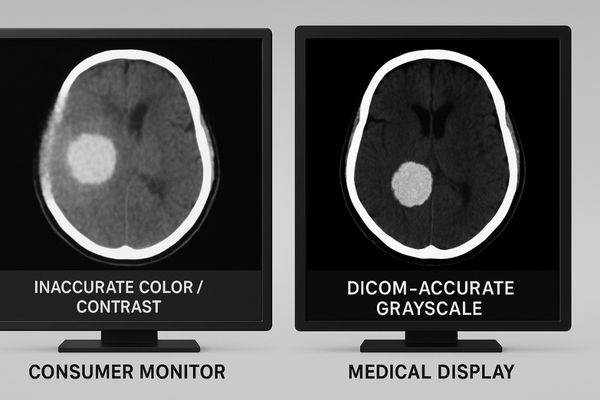
While a consumer 4K monitor and a medical 4K monitor may share the same number of pixels, they are fundamentally different tools built for different purposes. A consumer display is designed to produce pleasing, vibrant images for entertainment. Its colors are often oversaturated, and its brightness and contrast are manipulated to look dramatic. This is the exact opposite of what is needed for medical diagnosis. A medical display is a scientific instrument. Its primary goal is accuracy and consistency. It undergoes a rigorous factory calibration process to ensure it conforms to the DICOM Part 14 standard7. This standard dictates precisely how every shade of gray should be displayed, ensuring that an image will look the same whether it is viewed in your hospital or a consulting specialist’s office across the world. Specialized displays also include sensors that constantly monitor and stabilize the backlight’s brightness, ensuring consistent image quality over thousands of hours of use. For imaging that requires both high resolution and precise color, such as PET/CT fusion or digital pathology, a monitor like our MD50C – 5MP Color Mammography Monitor8 provides the necessary fidelity that a consumer display simply cannot match.
Medical Display vs. Consumer Display
| Feature | Specialized Medical Display | Standard Consumer Display |
|---|---|---|
| Calibration | Factory calibrated to DICOM Part 14 standard | Not calibrated for medical use; optimized for visuals |
| Brightness | High, stable, and uniform across the screen | Variable; often has bright spots and dim corners |
| Grayscale | Precise and consistent grayscale rendering | Inaccurate grayscale; details in dark/bright areas are lost |
| Longevity | Designed for long hours of use with stable performance | Performance degrades quickly with continuous use |
| Compliance | Meets regulatory standards for medical devices | No medical certifications |
Does increased resolution directly correlate with improved surgical planning and outcomes for oncology patients?
The ultimate goal of cancer surgery is to remove the entire tumor. An incomplete resection due to unclear margins often leads to local recurrence and poorer outcomes for the patient.
Yes, increased resolution directly correlates with improved surgical planning and better potential outcomes. Clearer visualization of tumor boundaries allows surgeons to define more precise resection margins, which helps in achieving complete tumor removal and preserving healthy tissue.
The information gathered from a high-resolution diagnostic image does not stay in the radiology reading room. It travels directly to the operating room, where it becomes the surgeon’s primary roadmap. When a surgeon can clearly see the full extent of a tumor and its relationship to nearby critical structures like blood vessels and nerves, they can plan a more confident and precise surgical approach. The goal in most cancer surgeries is to achieve "negative margins," meaning the tissue removed has a border of healthy cells all the way around the tumor. High-resolution imaging is a key enabler of this goal. In modern, technology-driven operating rooms, this planning is often done on 3D reconstructions9 of the patient’s anatomy. The quality and reliability of these 3D models are entirely dependent on the resolution of the original scans. During minimally invasive or robotic surgery, the surgeon relies exclusively on the image on the screen. A 4K surgical display, such as our MS321PB – 32" 4K Surgical Monitor, provides the depth perception and detail needed to manipulate instruments with precision, helping ensure that all malignant tissue is removed while sparing as much healthy tissue as possible.
Conclusion
In oncology, higher resolution is not a luxury. It is a clinical requirement that directly enhances diagnostic accuracy, enables more precise surgical planning, and ultimately contributes to better patient outcomes. To secure high-resolution medical displays for oncology applications, contact Reshin at martin@reshinmonitors.com.
-
Understanding the role of medical displays can enhance your knowledge of their impact on cancer diagnosis and treatment. ↩
-
Exploring this topic will reveal how crucial display resolution is for accurate tumor identification and surgical planning. ↩
-
Explore how high-resolution monitors enhance image clarity, crucial for accurate diagnosis in medical imaging. ↩
-
Learn about the significance of micro-calcifications in breast cancer detection and how they impact patient outcomes. ↩
-
Explore how a 5MP display enhances diagnostic accuracy and workflow efficiency in medical imaging. ↩
-
Understanding the imaging chain is crucial for ensuring high-quality medical images and effective diagnosis. ↩
-
Understanding the DICOM Part 14 standard is crucial for ensuring accurate medical imaging, which can significantly impact patient diagnosis and treatment. ↩
-
Exploring the advantages of a 5MP Color Mammography Monitor can reveal how it enhances diagnostic accuracy and improves patient outcomes in medical settings. ↩
-
Learn about the role of 3D reconstructions in surgical planning and their impact on patient safety and surgical success. ↩



