Medical teams regularly report inconsistent tissue color between camera feeds and displays, potentially compromising clinical decisions during critical procedures. Could your visualization systems be introducing unnecessary diagnostic uncertainty?
Accurate color reproduction is essential for endoscopy, surgery, and medical imaging workflows. In this guide, I break down how BT.709 and BT.2020 influence clinical visibility, why medical-grade displays matter, and what engineering principles ensure consistent color performance in real-world hospital environments.

As an engineer specializing in the calibration of medical displays, I’ve witnessed firsthand how color accuracy directly impacts clinical decision-making.
Throughout my career implementing visualization systems in operating rooms and imaging departments, I’ve consistently found that many facilities underestimate the engineering complexity behind reliable medical color reproduction.
This guide examines why color accuracy matters in healthcare environments, how industry standards like BT.709 and BT.20201 apply to clinical workflows, and what technical factors healthcare facilities should evaluate when selecting displays for color-critical applications. For OR managers, imaging directors, and biomedical engineers responsible for visualization infrastructure, these considerations directly influence clinical confidence and workflow predictability.
What Does "Color Accuracy" Mean in Medical Displays?
Healthcare facilities often struggle with inconsistent color presentation across different screens and devices, creating confusion about what represents the "true" tissue appearance. What exactly constitutes "accuracy" in medical visualization?
In medical display calibration, I rely on accuracy defined by signal fidelity—ensuring the display reproduces the imaging modality’s intended colors consistently, without enhancement, drift, or misleading shifts. Medical-grade displays maintain this fidelity through precise gamma control, stable backlights, and strict white-point management.
Color accuracy in medical displays encompasses several interrelated technical concepts that collectively determine clinical reliability.
Color Fidelity vs. Visual Appeal
A fundamental distinction exists between displays optimized for consumer entertainment and those engineered for clinical use.
Consumer displays typically enhance colors to create visually appealing images with increased saturation and contrast. These enhancements may look impressive but distort the original image data.
Medical color accuracy2 prioritizes faithful reproduction of the source signal. This fidelity matters because tissue color represents a diagnostic indicator, treatment decisions rely on subtle color variations, and clinical documentation requires reproducible results.
In my calibration projects, I often encounter newly installed systems where commercial-grade monitors render the same endoscopic feed with dramatically different color temperatures and saturation levels than medical displays. These variations may appear aesthetic but can mislead clinical interpretation.
Measurable Components of Medical Color Accuracy
Color accuracy can be quantified through:
| Component | Definition | Clinical Significance |
|---|---|---|
| White Point | Color temperature of “white” | Impacts all color perception |
| Delta-E | Measured difference between intended vs. shown color | <2.0 ideal for clinical use |
| Color Gamut | Total color range a display can reproduce | Must match source modality |
| Color Uniformity | Consistency across the screen | Prevents region-based misinterpretation |
| Gamma | Signal–brightness relationship | Controls midtone detail visibility |
These parameters must be measured during installation and periodically across the lifecycle—not by visual impression alone.
Why Are BT.709 and BT.2020 Critical for Surgical and Imaging Workflows?
Medical facilities increasingly report compatibility issues between older and newer imaging systems, creating workflow disruptions. How do standardized gamuts address this?
BT.709 and BT.2020 define the color gamuts used throughout medical imaging. In my OR deployments, BT.709 remains the foundation for consistent HD color reproduction, while BT.2020 enables wider, more precise chromatic detail in advanced 4K/8K systems—provided the full imaging chain maintains clinically neutral mapping.
Color gamut standards create a unified framework for consistent reproduction across the imaging chain.
The Evolution from BT.709 to BT.2020
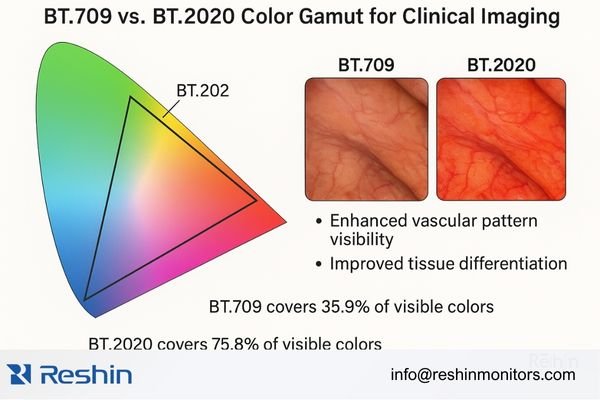
BT.709 (Rec.709) is the standard gamut for HD video including most existing endoscopic systems. BT.20203 (Rec.2020) significantly expands color range for 4K/8K ultra-high-definition imaging.
Key differences include:
- BT.709 covers ~35.9% of visible colors; BT.2020 covers ~75.8%
- BT.2020 defines more saturated primaries
- Wider gamut improves visualization of clinically relevant color subtleties
More hospitals now operate hybrid environments where BT.709 and BT.2020 coexist—making accurate mapping essential.
In practice, BT.709 remains the baseline for HD medical visualization, while BT.2020 should be implemented only when the entire imaging chain can maintain clinically neutral wide-gamut output.
Clinical Implications Across Specialties
- Endoscopy & MIS: BT.709 remains dominant, while BT.2020 enhances vascular pattern clarity in advanced 4K scopes.
- Pathology & Dermatology: Wider gamuts improve interpretation of stained tissues and subtle skin tone variations.
- Radiology: While mostly grayscale, modalities like nuclear medicine and 3D post-processing rely on accurate color maps.
How Do Color Gamuts Affect Clinical Visibility and Decision-Making?
Clinicians frequently report that certain structure details appear on one display but not on another. Why?
From an engineering standpoint, wider color gamuts reveal subtle vascular structures, mucosal differences, and inflammation cues that narrow gamuts may hide. However, without calibration, wide gamuts can distort tissue tones—so clinical neutrality, not vibrancy, is the goal.
Different tissue types produce characteristic color signatures. These include vascularity variations, mucosal tone shifts, inflammation gradients, and early necrotic changes.
A display’s gamut directly affects visibility of these cues. In my calibration work, wider but clinically neutral gamuts consistently produce more distinguishable boundaries between tissue types—critical in MIS procedures where tactile feedback is minimal.
Modern displays also incorporate color enhancement tools4 such as dynamic enhancement, procedure-specific modes, and adaptive gamut mapping. However, these must be balanced carefully. Excessive enhancement introduces artificial cues; insufficient enhancement hides clinical detail.
What Engineering Factors Influence Color Accuracy Over Time?
Healthcare facilities often find that initially accurate displays gradually drift. What causes this?
Long-term color accuracy depends on how well the display compensates for backlight aging, panel drift, temperature shifts, and environmental impacts. Medical-grade displays use stabilization sensors, uniformity correction, and auto-calibration to preserve reliable color output across years of clinical operation.
Backlight degradation is a primary factor. LEDs lose brightness 15–30% in the first 10,000 hours, causing color temperature shifts. Uneven aging further disrupts RGB balance5.
Reshin’s medical displays implement backlight stabilization using internal sensors to correct output drift. During long-term OR deployments, I routinely see Reshin systems maintain accuracy within ±5%, while consumer displays often drift beyond 20%.
Environmental conditions also affect stability. Temperature shifts, ambient lighting, cleaning chemicals, and 24/7 usage all degrade optical performance. Advanced medical displays counter this with temperature sensors, ambient compensation, self-calibration cycles, and durable optical surfaces.
In my deployments using Reshin systems, these compensation features have consistently maintained tight color tolerances across years of heavy clinical use.
How Should Hospitals Evaluate Color Accuracy When Selecting Displays?
Procurement teams often rely on marketing specs or visual demos that don’t reflect real performance. What should they test instead?
For clinical evaluation, I prioritize objective measurement—Delta-E, white-point drift, uniformity variance, and BT.709/BT.2020 coverage—combined with system compatibility checks and long-term calibration support from the display vendor.
Objective evaluation must include:
- Color accuracy verification via spectrophotometer
- Uniformity testing across multiple screen points
- Stability comparison after warm-up and extended use
- Gamut coverage confirmation for BT.709/BT.2020
System-level validation requires checking compatibility across the entire imaging chain—including cameras, processors, and routing.
For procurement teams, the essentials are objective measurement reports, system compatibility with your imaging devices, and a vendor’s long-term calibration support commitment.

Recommended Models for High-Accuracy Medical Color Reproduction
Healthcare facilities face increasingly complex choices when comparing medical displays from different vendors. Which displays deliver reliable color accuracy while still fitting into real-world surgical and imaging workflows?
As a Reshin engineer, I focus on models that combine precise BT.709/BT.2020 handling with practical OR and radiology integration. Across my surgical and imaging deployments, these Reshin displays have shown stable, clinically neutral color performance that distributors can confidently position in tenders and hospital standardization projects.
| Model | Key Specifications | Optimal Applications | Color Performance |
|---|---|---|---|
| MS275PA | 27" 4K Surgical Display | MIS, endoscopy | BT.709 calibrated + optical bonding |
| MS322PB | 32" 4K OR Display | Hybrid OR | Wide-gamut processing + AR glass |
| MS430PC | 43" 4K Large-format OR Display | Teaching, multi-viewer environments | Strong BT.2020 support |
| MD32C | 32" Diagnostic Color Display | Radiology, clinical review | Stable BT.709 color accuracy |
| MD85CA | 32" High-Resolution Diagnostic Display | Pathology, advanced visualization | High-precision BT.709 color performance |
Standardizing on a consistent display family improves color consistency, user confidence, and maintenance efficiency across clinical areas.
These recommendations are based on real deployments of Reshin monitors in ORs and imaging departments where color accuracy directly impacts clinical performance.
FAQ: BT.709, BT.2020 & Medical Display Color Accuracy
Do all medical displays need BT.2020 support?
No. In my engineering work, I still see BT.709 as the main “baseline” for most surgical and radiology workflows. If the cameras, routers, recorders and PACS systems are all BT.709, forcing BT.2020 on the display side doesn’t create new clinical information—it just complicates calibration and acceptance testing. BT.2020 only becomes meaningful when the entire imaging chain, from acquisition to viewing, is designed, calibrated and verified for wide-gamut operation.
When is BT.2020 actually useful in clinical environments?
BT.2020 starts to add real value when advanced cameras and imaging systems are already producing wide-gamut content and the hospital has a clear use case for subtle color differences—typically high-end minimally invasive surgery, pathology-style visualization, or multi-modality review where color nuances matter. In those cases, I design the chain so that BT.2020 signals are preserved end-to-end, then use strict calibration and profiles to keep colors clinically neutral rather than “demo vivid”.
Why can BT.2020 make surgical images look “too red”?
In practice, I often see BT.2020 used with consumer-style “vivid” presets rather than clinical calibration. The wider gamut gives more room for saturated reds and pinks, so if the lookup tables and white point are not tuned for medical use, vessels and tissue can look unnaturally intense. This is why I treat BT.2020 as a capability, not an automatic upgrade: without proper calibration targets, verification tools, and consistent profiles across devices, BT.2020 can distort clinical judgment instead of improving it.
Can consumer 4K TVs replace surgical displays if they advertise BT.2020?
No. Even if a consumer TV claims BT.2020 support, it is not engineered for medical use. From an engineering standpoint, medical displays add multiple layers that TVs don’t provide: stable luminance control over long shifts, repeatable calibration modes, tighter tolerances for grayscale and color tracking, and firmware designed for predictable behavior in OR or reading-room environments. They also integrate with hospital safety, cleaning and quality-control protocols. For these reasons, I never recommend consumer 4K TVs as substitutes for certified surgical or diagnostic displays.
How should hospitals and distributors evaluate color accuracy in tenders?
When I help evaluate color-related tender requirements, I look beyond “BT.709/BT.2020 supported” checkboxes. I focus on whether the vendor can provide: documented calibration workflows, measurement reports or factory calibration data, stable behavior over time (warm-up, drift, aging), appropriate presets for specific modalities, and clear guidance on how to verify performance on site. A display that combines proven BT.709 accuracy with carefully controlled BT.2020 handling, plus practical calibration and QA procedures, will usually be a safer choice than a product that simply lists wide-gamut support on the spec sheet.
Conclusion
Color accuracy in medical displays influences clinical interpretation, diagnostic confidence, and ultimately patient outcomes. BT.709 and BT.2020 provide the foundation for consistent color reproduction, but engineering factors such as backlight stability, uniformity correction, and long-term calibration determine whether a display maintains clinical reliability over time.
In my experience implementing visualization systems across hospitals, displays engineered specifically for medical environments consistently outperform consumer models. Reshin’s surgical and diagnostic displays integrate calibrated color modes, advanced stabilization systems, and clinically validated color engines to support precise visualization in demanding environments.
If your team is currently reviewing medical display performance or preparing for a visualization system upgrade, our engineering team at Reshin would be glad to provide technical guidance, model recommendations, or on-site evaluation to support your planning process.
📧 info@reshinmonitors.com
🌐 https://reshinmonitors.com/
-
Exploring these standards will enhance your knowledge of display technology and its impact on healthcare. ↩
-
Understanding color accuracy is crucial for medical professionals to ensure precise diagnostics and treatment decisions. ↩
-
Explore how BT.2020 enhances color accuracy and visualization in medical imaging, crucial for effective diagnosis. ↩
-
Exploring color enhancement tools can improve visualization and accuracy in medical procedures. ↩
-
Exploring RGB balance will enhance your knowledge of display technology and its impact on visual performance in medical settings. ↩



