In modern healthcare environments, the challenge of ensuring reliable display connectivity across multiple vendor systems has become increasingly complex, with clinical teams depending on seamless visual integration for critical decision-making.
Signal input compatibility in medical-grade monitors requires a systematic engineering approach that addresses EDID management, signal timing standardization, and topology planning. Success depends on locking down validated profiles, controlling negotiation behaviors, and implementing redundant routing paths to ensure predictable performance across multi-vendor environments.
As a systems engineer working on medical display integration, I’ve seen “plug-and-play1” assumptions break down once the same sources and displays are routed through real distribution chains across multiple rooms. In practice, compatibility means predictable lock time, stable image continuity, and repeatable switching behavior—even when devices from different vendors interpret standards and handshake states differently.
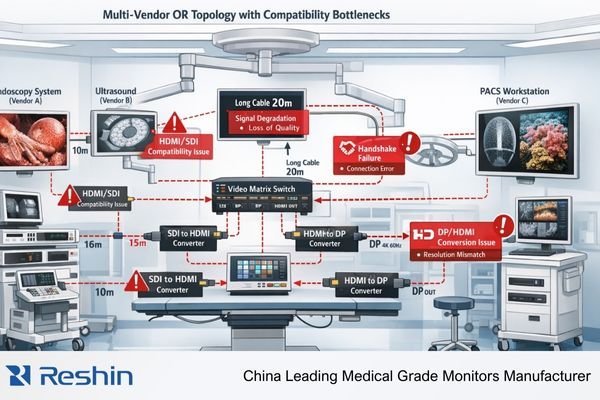
What breaks input compatibility in multi-vendor medical display systems?
The complexity of modern healthcare imaging demands robust signal connectivity, yet the interaction between different vendors’ equipment often reveals hidden compatibility challenges.
Input compatibility failures typically occur at interface boundaries where seemingly identical signal formats encounter varying implementations of EDID handling, HDCP states, and timing tolerances. These differences manifest as black screens, slow source switching, intermittent signal drops, or inconsistent image quality across rooms.
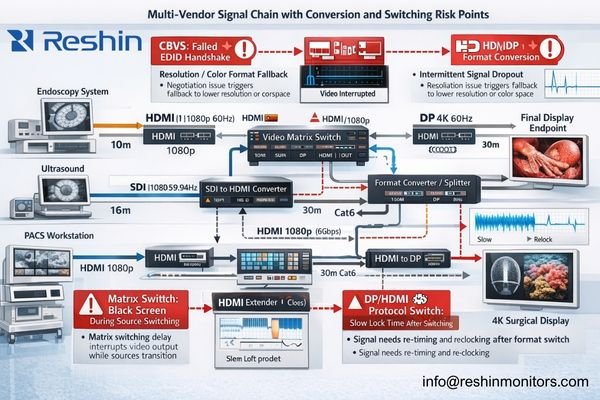
Compatibility failures in multi-vendor environments usually cluster into two categories: protocol interpretation and distribution-chain amplification2. The most difficult cases are not “one bad device,” but small mismatches that only surface under switching, peak bandwidth, or when endpoints appear/disappear during maintenance.
Signal Protocol Mismatches
Protocol-level conflicts arise when devices interpret standard specifications differently. Typical triggers include EDID communication inconsistencies, unstable hot-plug behavior, mismatched HDCP states, and format negotiation drift (RGB vs YCbCr, subsampling, bit-depth fallback). In operating rooms, these issues show up immediately as unpredictable switching recovery, unexpected resolution fallback, or inconsistent color/bit-depth between rooms that were intended to be identical.
System Architecture Vulnerabilities
Signal margin and timing stability can compound across complex distribution chains. Each conversion boundary, matrix switch hop, extender stage, or reclocking point can change negotiation behavior or reduce link headroom—especially when multiple vendors’ devices are mixed without a validated “known-good” baseline and commissioning criteria.
How do HDMI and DisplayPort negotiation behaviors affect compatibility?
Signal negotiation behaviors vary significantly between interface standards, creating unique challenges for medical imaging environments where stability is paramount.
HDMI and DisplayPort each present distinct compatibility challenges in medical display systems. HDMI’s reliance on EDID and hot-plug behavior can create instability during switching, while DisplayPort’s link training and AUX-channel negotiation add complexity to multi-hop distributions.
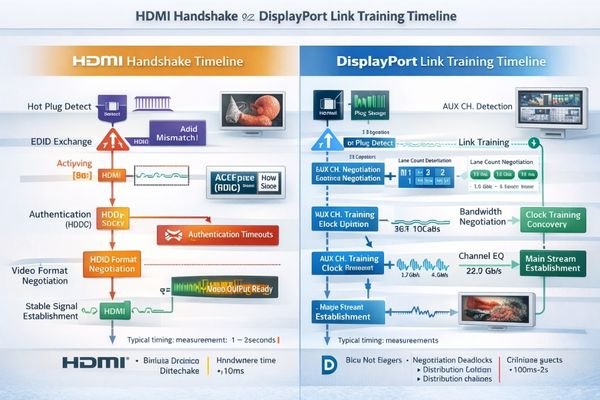
In PACS, KVM, and OR distribution projects, the most reliable outcomes come from treating negotiation as a controlled system behavior rather than an automatic convenience. HDMI compatibility3 often improves when EDID is made consistent and hot-plug events are prevented from propagating unpredictably through the chain. DisplayPort environments benefit from constraining topology changes, minimizing ambiguous multi-hop paths, and verifying retraining behavior under worst-case switching conditions. Contact our engineering team for a protocol-path review.
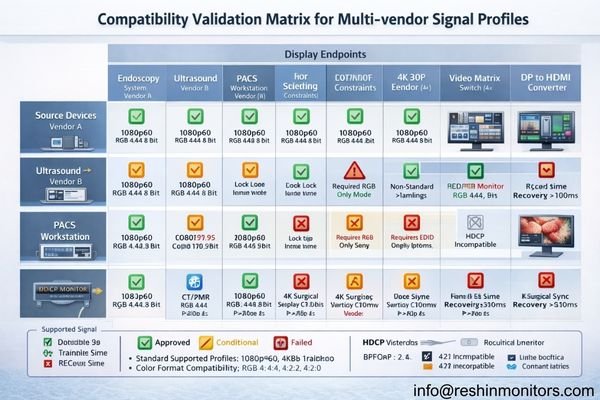
Which signal standards and profiles should be locked for predictable interoperability?
Standardizing signal profiles across multi-vendor systems requires careful balance between flexibility and reliability.
To ensure predictable interoperability, medical display systems should enforce a consistent set of validated signal profiles—resolution/refresh targets per workflow, standardized color policies (often RGB 4:4:4), defined bit-depth expectations, and explicit HDR/HDCP rules. A “golden EDID” approach creates a known-good baseline that can be commissioned and repeated across rooms.
Signal Profile Standardization Overview:
| Parameter | Common validated baseline | Validation requirements | Implementation notes |
|---|---|---|---|
| Resolution/Timing | Common starting points such as 1920x1080p60 and 3840x2160p60 | Verify stable lock and switching recovery across all sources | Prefer a small approved set; lock preferred timing in EDID |
| Color Format | Often RGB 4:4:4, 8/10-bit (workflow-dependent) | Confirm no unexpected color conversion or fallback | Avoid unintended YCbCr/subsampling unless required |
| HDCP Handling4 | Typically disabled unless explicitly required | Document exceptions and test full chain behavior | Treat as a policy decision, not a surprise handshake event |
| Audio/Auxiliary | Often disabled if unused | Verify no side-effects on video negotiation | Remove or de-prioritize in EDID when appropriate |
The engineering goal is not “support everything,” but “support the right set consistently.” A smaller, validated profile set is usually easier to commission, easier to maintain, and far less likely to break when a single vendor device is upgraded or replaced.
How should integrators architect multi-vendor routing to minimize outages?
System architecture decisions significantly impact the long-term stability and maintainability of medical display networks.
Effective multi-vendor routing architecture requires controlled conversion boundaries, deterministic switching behavior, and redundant routing paths for critical viewing positions. Stability improves when signal conditioning is placed deliberately, and when EMI- and grounding-risk zones are addressed with appropriate transport choices.
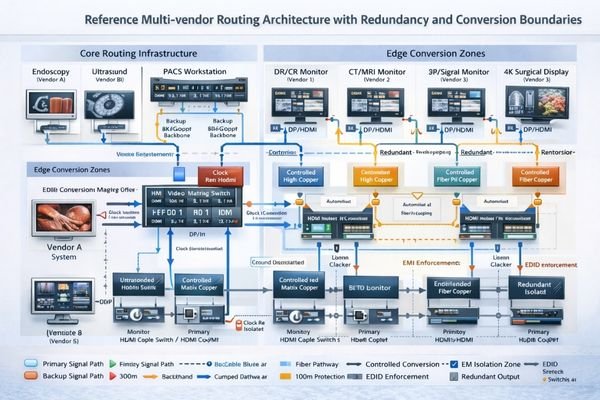
Signal Path Design
A resilient design constrains where format changes can occur and reduces uncontrolled multi-hop chains. In practice, that means defining clear “edge conversion5” zones, placing reclocking/retiming where bandwidth and distance make margin tight, and preferring fiber through EMI-heavy corridors or where ground potential differences can destabilize copper-based links. The design should explicitly state which profiles are allowed on which segments and how EDID is enforced end-to-end.
Redundancy Implementation
Critical viewing positions benefit from redundancy that is planned at the routing layer rather than improvised at the bedside. A secondary path (or a secondary input) is only useful if it is commissioned with the same validated profiles and if failover behavior is predictable under real switching conditions. For long-term reliability, the acceptance criteria should define switching recovery expectations and ensure the system remains repeatable after maintenance.
Which Reshin medical display models fit multi-vendor input compatibility planning?
The growing complexity of medical imaging environments requires displays that can maintain stable performance across diverse system architectures.
When planning multi-vendor integrations, I prioritize endpoint repeatability, serviceability, and the ability to standardize commissioning across rooms. Reshin’s medical display portfolio supports these priorities when the system design locks validated profiles, controls negotiation behavior, and treats routing and redundancy as part of the compatibility plan.
| Clinical Role / Application | Usage Pattern | Display requirements | Recommended Model | Key integration considerations |
|---|---|---|---|---|
| Primary Surgical Display | Constant viewing, critical timing | Predictable lock and switching behavior | MS321PC | Align to golden EDID baseline; validate worst-case switching |
| OR Overview Monitor | Multiple source switching | Fast, repeatable recovery | MS430PC | Verify deterministic switching behavior through the full chain |
| Teaching/Conference Display | Frequent format changes | Stable operation across approved profiles | MS550P | Constrain approved profiles to avoid uncontrolled fallback |
| Auxiliary Clinical Review | Simple, direct connections | Reliable endpoint behavior | MS270P | Reduce conversion hops; keep paths bounded and serviceable |
| Hybrid OR Integration | Complex routing requirements | Multi-input flexibility | MS322PB | Plan redundancy at routing layer; document known-good profiles |
FAQ
Who should “own” EDID in a multi-vendor room—source, matrix, extender, or display?
In most multi-vendor deployments, EDID should be controlled at the point that best stabilizes the entire topology—commonly the matrix/switcher or a dedicated EDID management layer—so sources see a consistent “golden EDID” regardless of which endpoint is active. The key is to define ownership explicitly, validate it with all devices, and document it for future maintenance.
Should HDCP be required, allowed, or explicitly disabled in medical workflows?
For many clinical workflows, HDCP is best treated as “explicitly disabled” unless a specific source requires it. Mixed or accidental HDCP behavior is a common cause of intermittent black screens and extended switching recovery, especially when recorders, converters, or secondary displays are present.
How can we prevent black screens and long lock times when switching sources?
Focus on deterministic switching behavior: lock EDID profiles, avoid unstable hot-plug propagation, constrain topology changes that trigger DP retraining, and validate switching under worst-case conditions (all endpoints connected, peak bandwidth, repeated switching cycles). The goal is repeatable recovery behavior rather than “it usually comes back.”
What input profiles should be standardized to ensure predictable interoperability?
Standardize a small set of validated profiles per workflow—timing targets, color policy (RGB vs YCbCr), bit-depth expectations, and clear HDR/audio rules—then enforce them consistently through the routing layer and EDID strategy. Fewer approved profiles typically produce better stability across vendors than trying to support every possible mode.
When should fiber extenders or reclocking be used to protect signal margin in EMI-heavy zones?
Use fiber when distance, EMI exposure, or ground-risk conditions make copper stability margins unreliable, and use reclocking/retiming where multi-hop distribution or bandwidth-critical segments can erode headroom. The decision should be based on the worst-case path and switching behavior, not just on a single “works once” bench test.
Conclusion
Successful multi-vendor medical display integration requires a systematic approach to signal compatibility: lock validated profiles, control negotiation behavior, constrain conversion boundaries, and commission the system against repeatable acceptance criteria. When compatibility is treated as an engineered contract rather than an assumption, stability improves across rooms and remains resilient through maintenance cycles.
At Reshin, we help teams define a golden EDID baseline, validate switching behavior across multi-vendor chains, and document a compatibility plan that stays stable as systems evolve. Contact our engineering team to review your multi-vendor compatibility design.
✉️ info@reshinmonitors.com
🌐 https://reshinmonitors.com/
-
Understanding the challenges of plug-and-play systems can help you avoid common pitfalls in medical display integration. ↩
-
Exploring distribution-chain amplification can provide insights into optimizing performance and reliability in your network. ↩
-
Explore this link to understand how to enhance HDMI compatibility, ensuring reliable connections and optimal performance in your projects. ↩
-
Exploring HDCP Handling strategies can clarify policy decisions and improve system compatibility. ↩
-
Understanding edge conversion is crucial for optimizing signal integrity and ensuring reliable performance in complex systems. ↩



